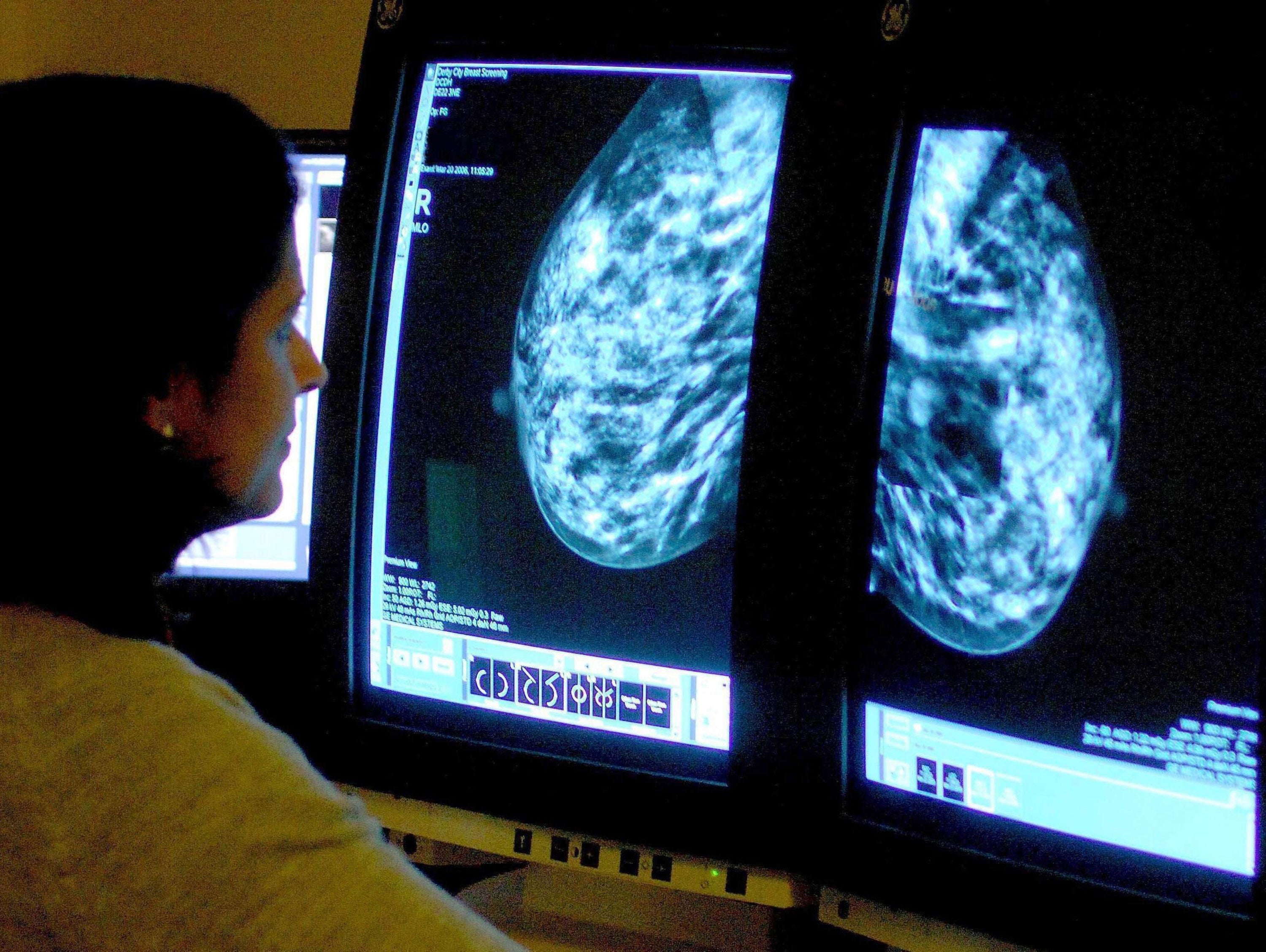
As a breast cancer survivor, I understand why women fear ‘wonder drugs’ like anastrozole
I worry that the focus on downsides will discourage women from even starting on this potentially life-giving medication, writes breast cancer survivor Leah Hardy

In September 2021, at the age of 58, I was diagnosed with an aggressive form of breast cancer. It was the most terrifying time of my life. I felt sure I was going to die and leave my two teenage children without a mother. Telling my family was heartbreaking, and then I faced months of intensive chemotherapy, life-changing surgery – including a double mastectomy – and 18 sessions of radiotherapy. I have been left with complications which mean I need at least another two operations over the coming year.
But I’m also pleased to say that, two years on, I’m considered cancer-free, and I feel good. But if I could have taken a daily pill to avoid getting cancer in the first place, would I have done so?
One such drug option is anastrozole. The hormone therapy has been used for years to treat breast cancer, and has now been licensed to prevent the disease from developing in the first place. Around 300,000 postmenopausal women in the UK with a family history of breast cancer are thought to be eligible. According to NHS England, even if only a quarter of these women opt to take it, anastrozole could prevent 2,000 of them from ever getting the shattering news that they have breast cancer.
A 2020 study published in The Lancet found that taking the oestrogen-reducing pill daily for five years slashed the risk of breast cancer by 54 per cent. And at just 4p per pill, compared to the thousands of pounds that cancer treatment costs, anastrozole is a bargain for the NHS.
You might think this is wholly wonderful news. But glancing at some quarters of social media, you might also think it’s a disaster, with people queuing up to regale women with tales of terrible side effects. One GP even posted on Twitter/X, that the side effects were so awful that no woman would be able to stay on the drug.
It’s true that anastrozole isn’t a magic bullet. Some women will still go on to be diagnosed with the disease and it’s only suitable for a minority of women.
And yes, like any medication, there are side effects. Anastrozole works by reducing the amount of the hormone oestrogen that a woman’s body makes, and while it will only be offered as a preventative to menopausal women – who already have low oestrogen – reducing the hormone even further can worsen many typical menopausal symptoms such as hot flashes. The drug can also cause joint pain and stiffness, rashes, nausea, headaches, depression and weaken bones. Women can’t take HRT while on anastrozole to mitigate any of these effects.
But it’s also important to remember that not all women will struggle. And I worry that the relentless focus on the downsides of treatment could dissuade some women who could benefit from anastrozole from even trying it.
Before I started chemotherapy, I read endless horror stories about it online. One account described it as “the nearest thing to dying without actually being dead”. People rushed to tell me that I’d feel (and be) sick, that I’d be exhausted and unable to do anything at home, that “everything you eat will taste awful,” that my toenails would drop off and my hair would definitely fall out, among many other grim tales. Looking at online forums connected to breast cancer charities, I saw some women were so terrified of chemo that many were thinking of refusing treatment altogether.
I even remember one woman on Twitter (as it was then) telling me that my treatment might not even work, and when I shared my joy that scans showed my cancer hadn’t spread to other organs and become incurable, answered “Not YET.” As a result of this negativity, I backed away from social media, horrified that what I hoped would be a supportive community sometimes felt like anything but.
But as it turned out, for me, chemo was fine. Not fun, but fine. Yes, I sometimes felt like a human pincushion, and I developed a minor blood clot in my arm. The “cold cap” I wore to try to keep my hair was pretty uncomfortable, and after numerous treatments, I developed brain fog which meant that words eluded me. But I was lucky – yes, lucky. For me, chemo didn’t feel anything like dying, and I think this experience should be as valid as the horror stories.
Even so, I would not give my cancer experience the full five stars on Tripadvisor. I sometimes miss my old boobs, and not working for a year was horrendous for our family finances. I still have to have at least two operations over the coming months to try to cure or ameliorate the side effects of my many treatments. I am also taking a drug – Zometa – to try to prevent cancer recurrence in my bones. Zometa carries its own risks, including the rare but devastating one of possibly making my jaw disintegrate. Does this worry me? Of course. But the prospect of cancer coming back worries me more.
As it happens, anastrozole would never have been an option for me. I have no family history of breast cancer, and my type of cancer – HER2-positive – is one of the 20 per cent of breast cancers diagnosed every year that are not fed by hormones.
But there are plenty of women who already take risk-reducing drugs – known as “chemoprevention” – despite their side effects. These drugs include other oestrogen-reducing drugs such as tamoxifen to reduce the risk of them coming back after treatment. And the fear of developing cancer, especially in women who have seen mothers, aunts and sisters struggle and even die of the disease, is such that some healthy women opt for drastic surgeries including radical hysterectomies and Angeline Jolie-style double mastectomies to try to dodge the cancer bullet.
One big reason why preventing breast cancer can be preferable to treating it once it appears is that, while in most cases women will be cured in around 20 to 30 per cent of women, the disease can recur in other organs, when it is known as secondary or metastatic breast cancer. This can happen up to 30 years after treatment and is considered incurable.
The bottom line is that no women will be forced to take anastrozole. It will only ever be an option that they can discuss with their doctors. There are non-hormonal treatments that can help with side effects such as hot flashes, local oestrogen for vaginal symptoms, and exercise can help with stiffness and joint pain.
And if side effects are still intolerable, women can, of course, choose to stop taking it. I worry that the focus on downsides will discourage women from even starting on this potentially life-giving medication.
Many breast cancer survivors say, quite rightly, that some menopause campaigning terrifies women because it can sometimes give the impression that life without HRT isn’t worth living. I think we need to be equally careful that we don’t end up scaring women off a potentially lifesaving drug that the charity Breast Cancer Now has described as a “major step forward”.
I know that going through treatment can be hard, but life is precious, and a diagnosis of breast cancer can be shattering. If I knew I was at high risk and could have taken something to stop that from happening to me, I think I would have. Your body. Your choice. All I’m saying is: let’s be careful about putting women off even trying something that could spare them from my ordeal.





