What we know about waning immunity and Covid booster jabs
The decision to roll out third doses on a mass scale has divided experts. So what does the science suggest? Samuel Lovett explains

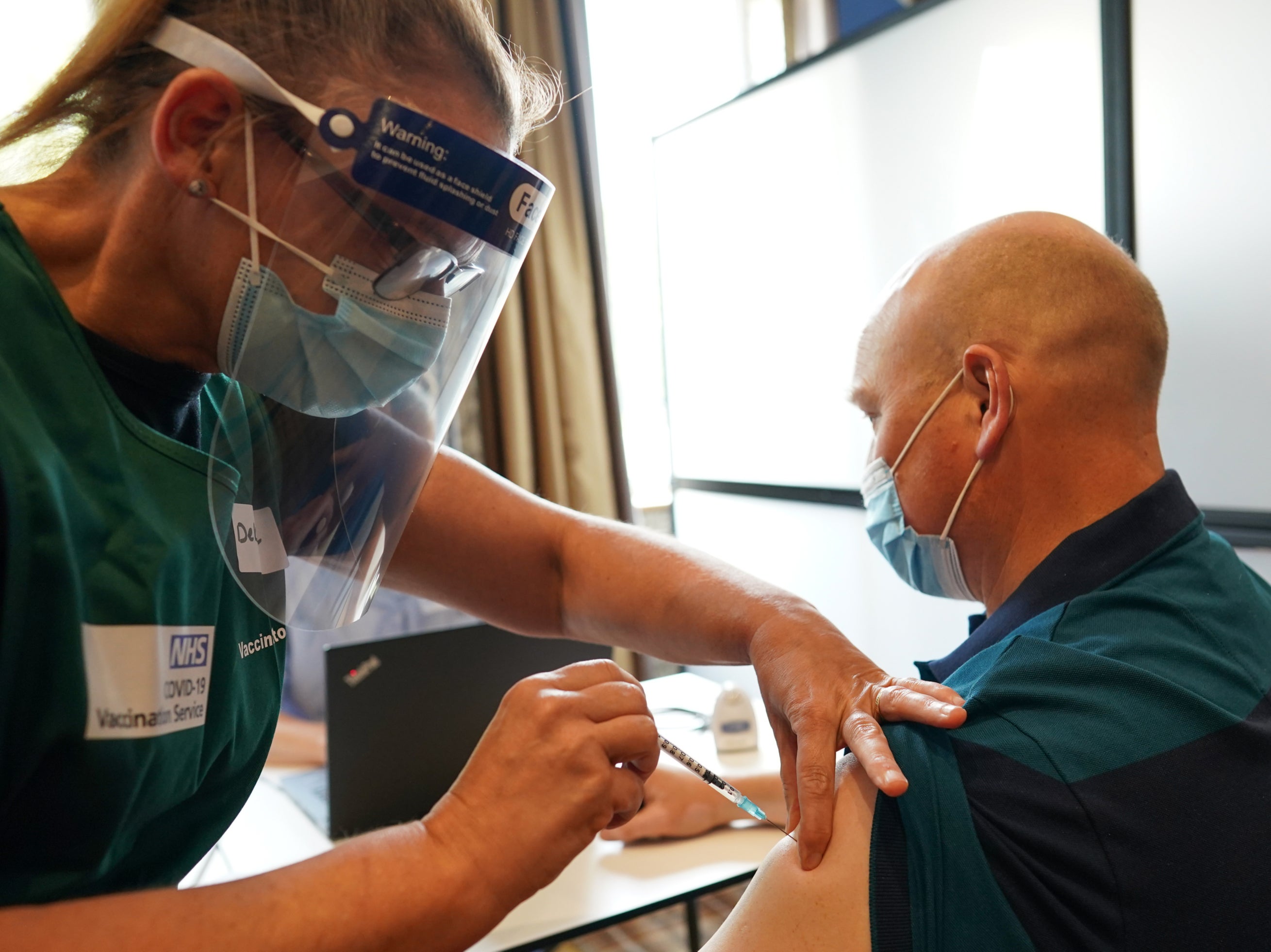
Britain has become the latest nation to announce its plans to roll out booster jabs, joining Israel and the US, amid fears of waning protection levels among the vaccinated.
The administration of a third vaccine dose for the over-50s will provide an immunological ‘top-up’ for these people, ensuring they remain protected against severe disease and hospitalisation.
The debate around whether or not booster jabs are necessary has raged for months, with many scientists arguing that the data isn’t clear enough to support these programmes – especially at a time when millions of people across the world remain unvaccinated.
At the beginning of the week, an international group of scientists, writing in The Lancet, condemned the mounting push for boosters in the West. Reviewing dozens of studies on the topic, the experts insisted the evidence isn’t strong enough to support mass booster programmes, concluding that the focus should be on using the world’s precious vaccines supplies to immunise the unprotected.
“Our primary goal here in this pandemic was, first of all, to avoid, to end all preventable deaths,” said Dr Soumya Swaminathan, chief scientist at the World Health Organisation and a co-author of the review. “And since we have the tools to do that very effectively, we should be using it to prevent deaths around the world.”
Others have argued that it makes sense to take the front foot against Covid-19, especially when there are signs that immunity levels are indeed waning in some groups.
Likening the UK’s booster programme to campers who prepare against an incoming storm, Professor Jonathan Van-Tam, England’s deputy chief medical officer, said it was “better to put some extra guy ropes” on the tent now than to “wait until it’s the middle of the night and it’s howling with wind and rain”.
Professor Keith Neal, an epidemiologist at Nottingham University, said there was a “good argument” for third doses as by the time it’s definitively known whether they are needed on a wider population level, “we could be in a mess”.
A new study released by Public Health England this week helps paint a clear picture of waning immunity and where boosters might fit into this.
Its findings clearly show falling rates of protection against symptomatic infection after 20 weeks for all over-16s who have been vaccinated with Pfizer and AstraZeneca. (Moderna hasn’t been used as long in the UK, so the data does not stretch over the same time frame.)
This waning effect is more pronounced in different age groups, and also depends on which vaccines have been administered. Those over-65s who had the AstraZeneca vaccine have 36.6 per cent protection against symptomatic disease after 20 weeks, compared with 55.3 per cent for Pfizer, the study says.
Under the government’s plans, all over-50s will be offered a third dose of the Pfizer vaccine – regardless of what they were originally vaccinated with – to get this figure back up to its previous heights.
Israel was the first nation to offer third doses to its population, and according to real-world data collected from the country, a third Pfizer dose six months after a second shot restores protection from infection to 95 per cent. This is specific to the Delta variant, too.
If the aim of the UK is to limit infections, boosting all over-50s will clearly have an impact – but as the country seeks to “live with the virus”, it is surely hospitalisation trends that are the most important measure, with the main goal to stop people falling desperately ill and burdening the NHS as it seeks to recover from the fallout of the pandemic.
Here, the PHE data also shows a fall in protection against hospitalisation among those vaccinated with Pfizer and AstraZeneca. Again, the drop-off is dependent on age, vaccine and underlying health conditions. For over-65s deemed clinically extremely vulnerable (CEV), protection drops to below 60 per cent 20 weeks after two AstraZeneca jabs, compared with 71 per cent for Pfizer.
Boosting these groups will, clearly, save lives. This is not in dispute. As such, the UK has set out its plans to offer a third dose to more than 500,000 people classed as CEV, such as the immunocompromised.
It is the individuals outside these groups, such as those in their fifties, where questions have been asked over whether or not they require a booster jab. Supporters of the programme have referenced the Israeli data showing a rise in severe illness among vaccinated people of all ages.
But when these figures are broken down by age, only people above 60 show a notable drop in efficacy against severe illness. In the case of the UK, the graphs above show that there is not much difference in protection levels against hospitalisation between all healthy over-16s and over-65s.
Scientists believe this could be linked to the fact that the UK opted to extend the gap between first and second doses to more than eight weeks, helping to generate a better, longer-lasting response. Israel, in contrast, kept its interval to three weeks.
Nonetheless, there is a fall observed in the different groups, and although protection remains exceptionally high with both vaccines, a decrease of a few percentage points will still have an impact on the number of people who end up in hospital – especially if cases are surging.
Presumably on the basis of the data presented by PHE, along with other studies, Chris Whitty, England’s chief medical officer, insisted that “the logic of boosters for the UK is clear and science-based”.
Other studies from the US have delivered similar findings, concluding that the ability of the vaccines to prevent hospitalisations dipped most noticeably in adults aged 75 and over.
The WHO, the Covax Facility and other expert voices have made clear their opposition to booster jabs. The focus, they say, and rightly so, should be vaccinating the unprotected. Conversely, there is a belief among some quarters that “you can do both”, as the chief medical adviser to President Joe Biden, Dr Anthony Fauci, said, in terms of boosting the vaccinated and also offering first doses to those in need.
But with the vaccination rate currently hovering around the 1 per cent mark for the world’s poorest countries, there’s little to suggest that this dual approach will succeed any time soon.




Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments