NHS England’s ‘robust plan’ is not enough to avert disaster this winter
The UK’s healthcare system is heading for an iceberg, writes Adrian Boyle – but there is still time to change course

I am very worried about winter.
That may be unusual to read at the end of July, but even now during the warmer months – when things are “supposed to be quieter” – emergency departments remain under immense pressure. In June alone, more than 100,000 patients waited 12-hours in an A&E. These are patients seeking “emergency” care.
From the data, we know that the majority of people who wait the longest are the least able to cope; patients who are elderly, or who have mental health issues – often both. These patients are being let down by an under-resourced and under-staffed emergency care system, despite the efforts of hard-working emergency medicine staff.
Last winter, readers will recall multiple images of ambulances queuing outside hospitals, and the stories of patients waiting for hours inside A&Es. While the images and stories may no longer be on the front pages, the crisis has not gone away. The fear is that things will be worse this year.
On Thursday, NHS England published what was trailed as a winter resilience plan containing “robust new measures”. We were hopeful this might be a plan which would succeed where so many previous incarnations have failed.
It wasn’t. There were small nuggets of good – early focus; a call-to-action for better communication and a joined-up approach; clearer roles and responsibilities across the whole healthcare system.
However, having analysed it in detail, I have little confidence that this plan will do very much at all to prevent queues of ambulances outside hospitals, or the shameful sight of patients waiting for hours on trolleys in the corridors in A&Es full to bursting.
In reality this plan contains nothing new (a point explicitly reiterated during the NHS England Board meeting on Thursday). Once again, it is just more words on paper and will be little comfort or use to the patients and their loved ones who will feel the impact most acutely during winter.
I have seen headlines suggesting that this plan will see 5,000 new beds and 800 new ambulances. This is just not the case. These were announced in January as part of the Urgent and Emergency Care Delivery Plan which has so far failed to have a meaningful impact in recovering emergency care.
The Royal College of Emergency Medicine has always tracked bed data published by NHS England, especially since the announcement of the new care delivery plan. Since then, we have lost 1,841 general and acute (G&A) beds. From October 2022, which was when NHS England subsequently said the plan was to be considered to have been first implemented, we have gained 918 G&A beds.
NHS England then changed the start date again, saying the pledge of opening 5,000 beds began in April 2022. Since that time, we have gained 1,580 G&A beds.
Even if you start counting nine months before the Urgent and Emergency Care Delivery Plan was announced, NHS England is less than a third of the way to reaching its goal.
The shortfall of beds, mixed with the inability of the wider system to discharge patients to safe and appropriate care, led to the gridlock our hospitals faced last winter. This gridlock was associated with more than 23,000 excess deaths.
Changing definitions of what constitutes a bed, mixing in “virtual beds”, counting beds in closed wards – these tactics are nothing but smoke and mirrors. The public – our patients – and our members deserve more transparency and less distortion.
Put simply, we need more beds for our patients, enough staff to care for the patients in those beds and, when those patients are well enough to leave hospital, we need efficient discharge processes. This includes adequate social care, so that the next patients who need those beds can have them.
The announcement by NHS England of a financial incentive for major A&Es to perform better is seriously concerning and will probably lead to wider healthcare inequalities and gaming of the system.
The most deprived areas of England often have communities with the greatest healthcare (and other) inequalities. Major A&Es in these areas, that desperately need more support through investment, staffing and resources, will struggle to access this capital. As such, the money will flow to the most affluent and least desperate areas.
To access the “financial incentive”, A&Es must meet two targets; 80 per cent of patients being admitted, transferred or discharged within four-hours, and completing 90 per cent of (category 2) ambulance handovers (which are those for serious conditions such as chest pain and strokes) within 30 minutes.
The financial incentive to meet the four-hour target may drive a prioritisation of treating and discharging the least serious patients first. This would leave the most vulnerable, typically the elderly and those in poor mental state, waiting for hours potentially on trolleys in corridors.
Everyone who works in healthcare wants what is best for patients and staff. We acknowledge the aim of the NHS letter, but it is not enough. Patients and staff deserve better. Our members – and their colleagues – are dedicated, passionate, caring professionals but they are tired, undervalued, under-funded, under-resourced and under huge amounts of pressure.
Winter 2022 should have been a ground-zero moment, and yet we are not seeing the necessary urgency to prevent another cold-weather crisis. This winter cannot be allowed to be as bad as last year – it will break the very people who keep this broken system creaking along.
We are blithely sailing towards an iceberg, and it would be morally wrong for us not to raise our concerns now while there is still time to make a difference. The government must commit to effective and meaningful action and adopt RCEM’s five priorities to #ResuscitateEmergencyCare. If it does not, then we will simply repeat the cycle of dangerous overcrowding and corridor care and face another devastating winter – and nobody wants that.
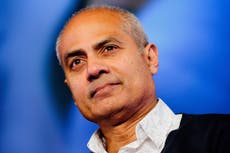
Dr Adrian Boyle is the president of the Royal College of Emergency Medicine
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments

Bookmark popover
Removed from bookmarks