Kawasaki disease: an unknown illness with no definitive medical diagnosis and no known cause – but it may all be in the wind
Kawasaki disease, an illness that can lead to heart disease in children, was first noted in 1871, but its cause is still unknown. Now, explains a former sufferer, scientists believe the answer may be blowing in Asia’s sand-laden winds

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
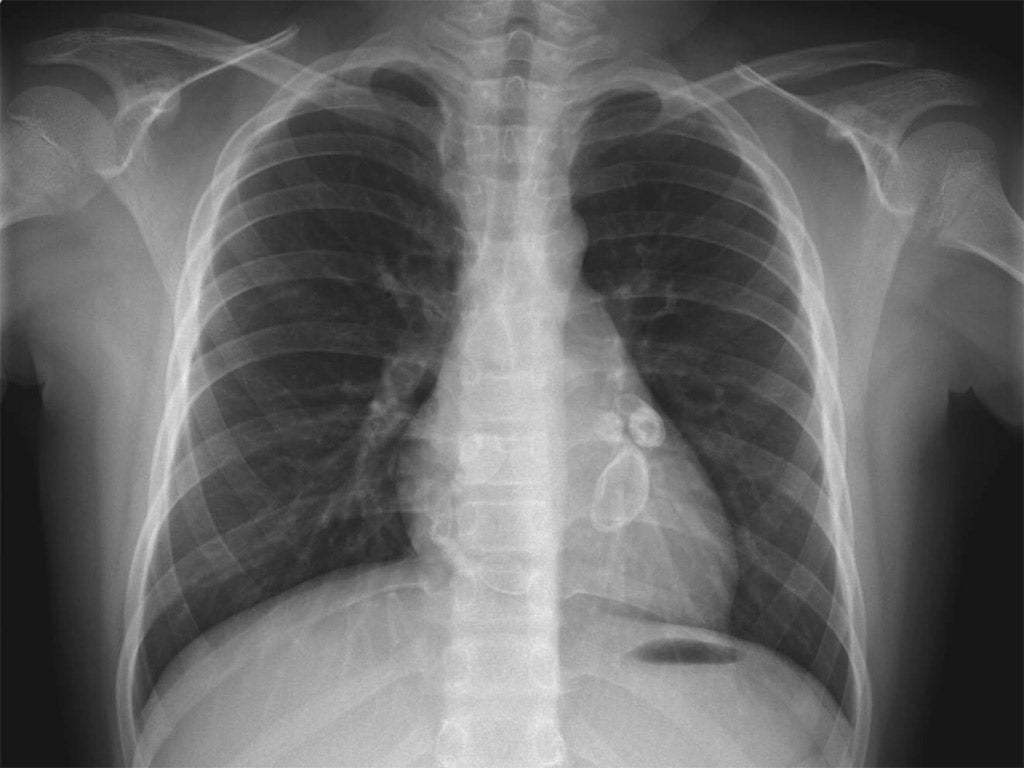
Your support makes all the difference.A child’s death from scarlet fever wouldn’t have raised any eyebrows during the devastating epidemics that swept Europe and North America in the 1800s. But Samuel Gee, a highly regarded doctor in England, found something very strange while cutting open the corpse of a seven-year-old boy in London in 1870. Gee’s post-mortem examination findings, preserved in a single paragraph written in 1871, recorded signs of damage called aneurysms in the coronary arteries running across the surface of the boy’s heart. In the affected regions, the main vessels that supply blood to the heart had expanded like balloons because of weakened vessel walls.
The case presented a puzzle to Gee, who commonly studied child patients while he worked at St Bartholomew’s in London. The boy’s medical history of having suffered a rash over his body would not have surprised Gee, as it was typical of scarlet fever, but heart disease in such a young child was simply baffling. Whatever the cause, it was beyond Gee’s Victorian-era medical knowledge.
Unable to solve the mystery, Gee did the next best thing: preserving the boy’s heart in formaldehyde and creating a medical curiosity for future generations in the process. The heart would float alone in its jar for more than 100 years before its significance was recognised – evidence of the earliest recorded case of Kawasaki disease in the world.
Alongside rheumatic heart disease, Kawasaki disease is the leading cause of acquired heart disease in young children in high-income countries. Modern medicine can treat most patients with Kawasaki if they are diagnosed early enough. But progress has been limited, and we still do not know what causes it. There have been many theories since the disease was first medically recognised by the Japanese doctor Tomisaku Kawasaki in 1967. Some researchers have pointed to an unknown virus. Others say it’s a bacterial or fungal toxin. In the 1980s, some medical experts suspected carpet-cleaning chemicals. Several groups have hypothesised that the disease is the result of agents that can trigger an overreaction of the immune system. Nobody has a satisfactory answer.
Kawasaki disease found me as an eight-year-old growing up in Cleveland, Ohio. An Asian-American boy with ancestral ties to Taiwan and China, I fit the typical patient profile. In the US, children of Asian descent have the highest rates of Kawasaki disease, followed by Afro-Americans, Hispanics and whites. The disease is more common among boys than girls. But I was somewhat older than the typical patient. Most are five or under, and the average age to have Kawasaki disease is two.
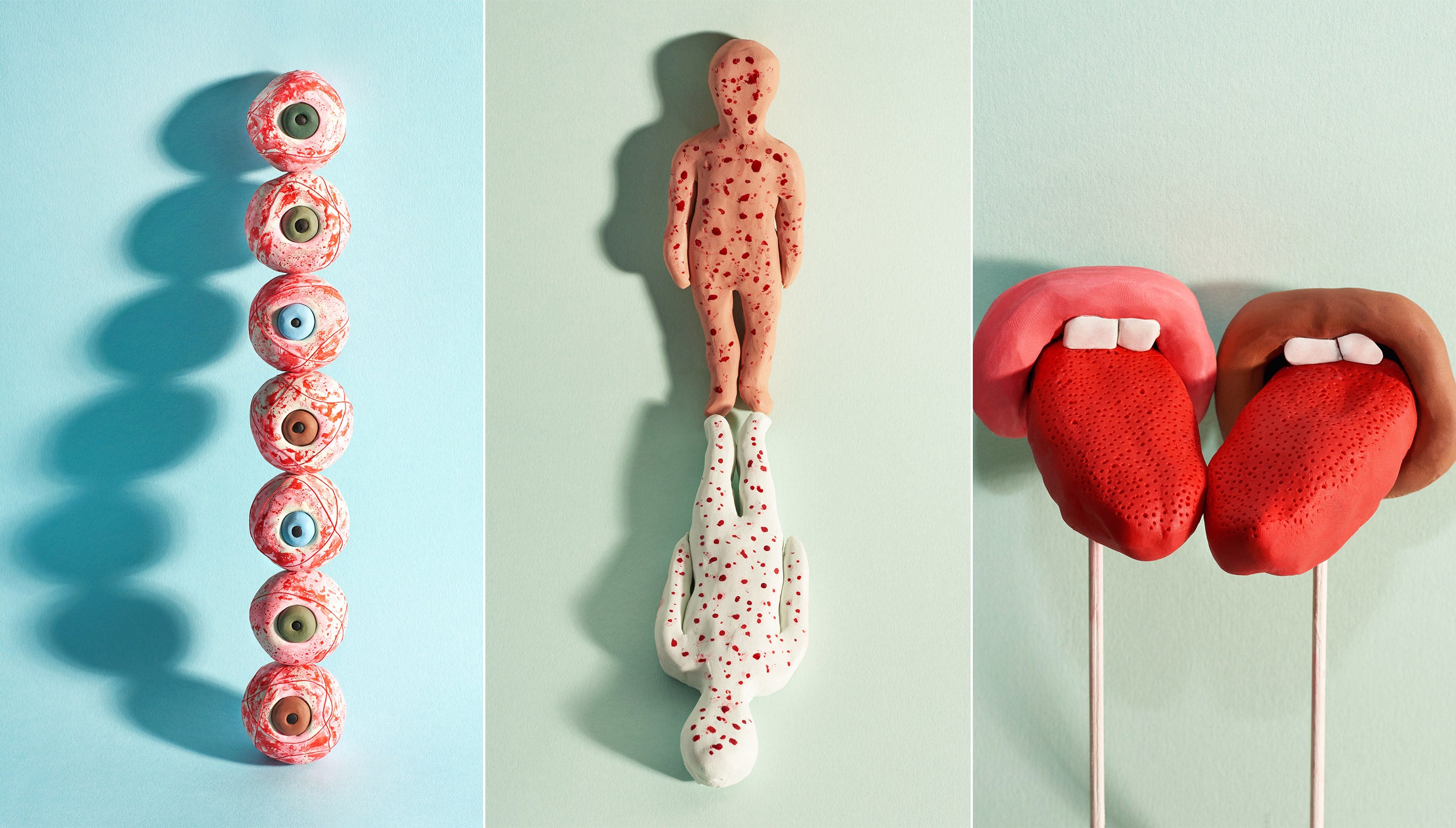
I developed the classic symptoms within a week. On Saturday, at the start of my illness, my parents took me to the doctor’s surgery to get tested for a bacterial infection. It came back negative. I soon became feverish. The lymph nodes on the sides of my neck became swollen. My tongue took on a strawberry appearance and my lips cracked. My fingers and toes began peeling. My eyes went reddish. I vomited. At one point, I felt too weak to walk upstairs to the first floor of my family home. I dropped to my hands and knees and crawled instead.
Five days after the start of my illness, paediatricians diagnosed me with Kawasaki disease. I was admitted to hospital on Thursday. By that time, I was complaining of aching joints and had developed a rash on my legs and ankles. My palms and feet were red and warm to the touch. Still, I was lucky. My doctors had dramatically boosted my chances of full recovery by diagnosing me within the first seven to 10 days, a crucial window for treating Kawasaki disease. The hospital stuck an intravenous needle into my arm to deliver a single large dose of gamma globulin, a type of immunoglobulin, which contains antibodies derived from plasma from many blood donations.
This treatment has proved effective in preventing most patients from developing coronary artery aneurysms – as about 20 per cent of untreated children will – which can lead to heart attacks and, very occasionally, premature death. But while intravenous immunoglobulin is the main treatment for Kawasaki disease, a small group of unfortunate patients don’t respond to the standard treatment and remain at risk of developing coronary aneurysms. Other therapies have been tried but remain unproven.
Although aspirin is not normally given to under-16s, children with Kawasaki usually get aspirin to bring down the fever and ease joint pain. When I failed to swallow some aspirin tablets and spat them out into my cup of water, the nurse on the night shift was not amused. I ended up having to drink my medicine as a bitter dose of aspirin-flavoured water. But my health was on the mend.
By Friday, I was eating sorbet and feeling much better. Troops of house doctors stopped by my hospital room to hear about my unusual disease from an attending specialist. By Saturday morning, I was allowed to go home. In the following months, echocardiogram tests showed that my coronary arteries had become only slightly enlarged as a result of the illness, before returning to normal size.
I had survived my encounter with Kawasaki disease. But, as I said, I was lucky. I fell ill at a time when more US doctors were recognising and diagnosing the disease, and when – just as importantly – they had learned, from Japanese colleagues, how to treat it.
I didn’t fully appreciate the psychological impact of Kawasaki disease until I attended a parents’ session at the Eleventh International Kawasaki Disease Symposium in Hawaii in early 2015. There I watched one young mother choke up with tears as she recounted her two-year-old son’s recent experience of Kawasaki disease. “It’s just so emotional,” she said. “My husband and I just don’t know anything.”
Another mother asked for help because her local doctors had failed to diagnose her son before he developed coronary aneurysms. “I don’t want to be left behind again,” she said.
Anxiety often grows as parents learn that it’s an unknown disease with no definitive medical diagnosis and no known cause, says Greg Chin, president of the Kawasaki Disease Foundation (which he helped to create after his firstborn son came down with it in 1998). When parents are told that the disease could potentially cause heart damage in their young child, the stress level “goes through the roof”.
Even if treatment proves successful, parents spend the following weeks checking the temperature of their child and wondering about the possibility of a relapse. The stressful period can stretch for months as follow-up echocardiograms check for any signs of coronary artery damage. In the rare worst cases, patients who develop coronary aneurysms may face a lifetime of uncertainty.
“It’s a terrible situation in the current century of medicine when you have to tell parents you know what’s wrong with their child, but you don’t know the cause of the illness,” says Anne Rowley, a specialist in paediatric infectious diseases. “We have a treatment but don’t know how it works. The child could be left with lifelong heart disease. This is what modern medicine has to tell them.”
Today, Japan has the highest rate of Kawasaki disease in the world, and the numbers keep rising. The annual incidence for the past few years has been well above 200 per 100,000 children under the age of five, reaching 264.8 children per 100,000 in 2012 (meaning that there were almost 14,000 cases that year). South Korea and Taiwan have the second- and third-highest rates of Kawasaki disease in the world.
The first modern cases outside of Japan were seen in Hawaii in the early 1970s. Today, it is the US state with the highest incidence of Kawasaki disease (about 50 cases per 100,000 children under five, compared with nearly 21 cases per 100,000 on the US mainland).
Seeing this pattern, some researchers began wondering if winds could be playing a role in the spread of Kawasaki disease; in particular the winds that create a seasonal phenomenon known as “yellow sand”, “Asian dust”, or variations of those names. Every spring, dust from the Gobi Desert in northern China and Mongolia enters the atmosphere and travels east to other parts of China, Japan and Korea. The dust sometimes picks up industrial pollution from China as it sweeps the land.
Xavier Rodó, a numerical ecologist and climatologist at the Catalan Institute of Climate Sciences in Spain, led the charge. He teamed up with Japanese and US colleagues to find out more, and they soon found a consistent pattern between seasonal shifts in the winds coming out of Central Asia and fluctuations in the number of Kawasaki disease cases in Japan, Hawaii and San Diego. The wind patterns even showed a possible connection with year-to-year variations in cases.
The next step involved pinpointing the source of whatever was being carried on the winds. Rodó and colleagues looked at the daily numbers of Kawasaki disease cases within individual Japanese cities and also focused on three major epidemics. Their results, published in 2014, pointed to a region in north-east China.

Patients seemed to develop the first signs of fever within a day of being exposed to whatever might be carried on the winds – far too short an incubation period for most known infectious agents, including viruses. The timeframe between exposure and illness suggests that Kawasaki disease may be an almost immediate bodily reaction, believes Rodó, triggered by something such as a bacterial or fungal toxin. Past studies have indicated a genetic susceptibility to Kawasaki disease within individual families and certain ethnic populations, which suggests that a person’s genetics plays a role in whether they’re susceptible to the toxin or not.
Rodó and his team need to expand their findings, but he is optimistic. They have already used aircraft to collect samples of the air above Japan, which have contained as many as 11 different species of the fungus candida, the most common cause of fungal infections in humans. The team eventually hopes to collect air and ground samples from north-east China.
If the theory is correct, China is almost certainly not the only source of any windborne agent, says Rodó. The existence of other sources would help explain the worldwide incidence of Kawasaki disease, which varies wildly from country to country. For instance, the latest figures show that South Korea has 134 cases of Kawasaki disease per 100,000 under-fives; Australia, nine; and England, eight.
Most researchers working on Kawasaki disease don’t try to propose all-encompassing theories about the cause of the disease. Instead, they focus on chipping away at the smaller unknowns in different ways.
Some researchers mimic the condition in genetically modified mice to study how immune-system responses damage the arteries; others use mice to begin examining the possible role of bacteria that live inside the gut. Genetic studies of humans have also helped identify specific immune-system signals and molecules that seem to play a role in the disease. Such research typically flies under the radar of both the media and the public.
By comparison, the windborne theory has earned an occasional flurry of media attention for Kawasaki disease over the past few years. But the truth is that it’s just one of several theories about the cause. Such theories continue to spark strong disagreement among Kawasaki researchers. For instance, most researchers I spoke with have adopted wait-and-see stances on the windborne theory, ranging from cautious to sceptical.
One of the more controversial ideas to come out recently is from Michael Portman, the director of Pediatric Cardiovascular Research at Seattle Children’s Hospital. In 2012, he published a study about how diets rich in soy might put children at greater risk of getting Kawasaki disease. It focused on how organic compounds found in soy, called isoflavones, could affect the immune system’s balance and inflammatory response.
A team of researchers in Toronto, Canada, meanwhile, is focusing on the idea that multiple agents are responsible. According to the hypothesis, these agents, be they infectious diseases or environmental factors, may modulate the immune response to make kids more or less tolerant to triggers. Other agents might be the triggers themselves.
While many researchers have given up on the idea of a virus being the main cause of Kawasaki disease, the Chicago-based doctor Anne Rowley isn’t one of them. She and her colleagues believe that the patterns of cases still point most strongly to some sort of respiratory virus, which infects many people when inhaled, but causes symptoms only in people with certain genetic vulnerabilities. Children may be most vulnerable because of the fact that their immune systems are still developing and they have lost protective antibodies that are passed on from their mothers during early life.

But identifying any potential virus remains difficult, because nobody has succeeded in fully replicating the disease in animal models or in cultured tissue, which means that researchers can’t just generate affected material in their labs for study. Instead, Rowley and her colleagues must manually track down cases of deaths caused by Kawasaki disease and ask for post-mortem samples. Despite the shortage of samples, Rowley’s group has managed to build a collection of heart specimens from more than 40 patients – some from post-mortem examinations, some from children who have received new transplanted hearts. The collection gives a sobering reality check of how extreme the consequences of Kawasaki disease can be.
The oldest known survivors of Kawasaki disease are now in their fifties. Nobody knows exactly what, if any, effects the disease has on life expectancy, but current evidence suggest that patients can expect to live normal lives if they haven’t suffered a large aneurysm. To help in the effort, as a survivor, I’m planning to participate in an adult Kawasaki disease survey being conducted at the University of California.
There’s no doubt that discovering the cause of Kawasaki disease could help in the development of more effective treatments. But Jane Burns, the director of the Kawasaki Disease Research Centre at the University of California, believes that solving the mystery will do more than just help the thousands of patients who suffer from the disease each year. It could radically change our scientific understanding of the way that human disease can develop.
Having seen her first cases of Kawasaki disease in 1978, Burns has been studying the possible causes of the disease for 30 years. Most recently, she has helped chase the windborne theory. “My hunch is that it’s not just going to be about the new virus or the new bacteria we didn’t know about,” she said. “It’s going to be a new story of how disease can be created in a subset of genetically susceptible people… a story of some new paradigm for triggering the body’s inflammation machinery.” But Kawasaki disease remains especially challenging to study because it’s a disease that affects relatively few patients.
Still, unexpectedly, the collection of hearts in Chicago is shedding light on the life – and death – of one young boy who died 145 years ago. Stanford Shulman, a Chicago paediatrician, stumbled across Samuel Gee’s lone paragraph about the mysterious case of the London boy while poking through some files in the 1970s. In the early 1990s, while stopping over in London during a sabbatical, Shulman made an appointment at the Barts Pathology Museum. He enlisted the help of his wife and the chief registrar in pathology at Barts to find the jar containing the boy’s heart.
“We can’t conclude with 100 per cent certainty that this child had Kawasaki disease,” Shulman says. “But it’s extremely likely he died from it, 100 years before Dr Kawasaki’s initial report of the same disease.”
Fifty years after Kawasaki gave his name to the disease, much has changed. More doctors know to suspect it in children with telltale symptoms that don’t respond to antibiotics or medicines to reduce fever. Hopefully that means more healthy survivors, such as me, and fewer young children’s organs in jars.
This is an edited version of an article first published on Mosaic and is republished here under a Creative Commons licence
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments