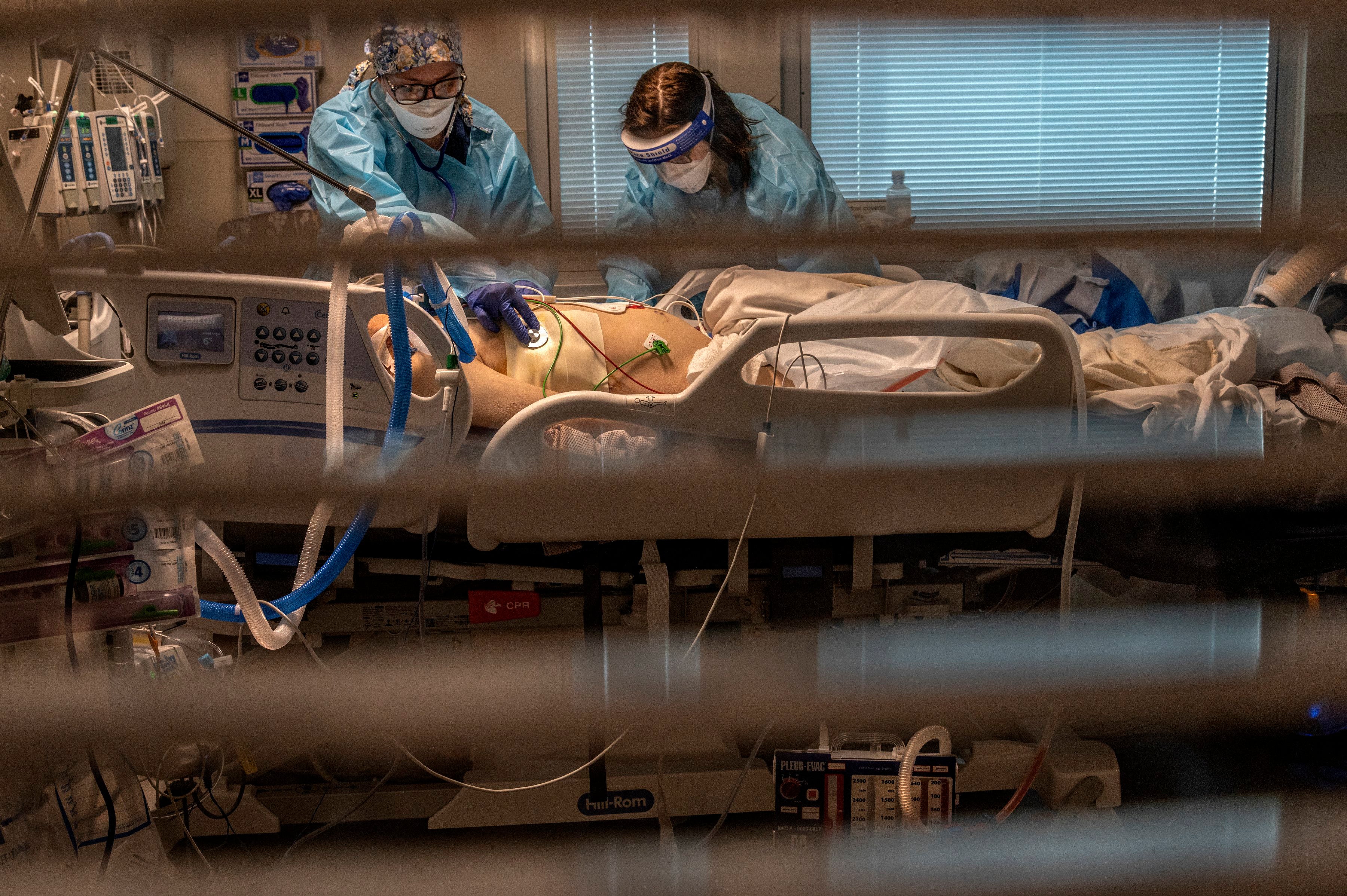
California health system buckling under strain of pandemic as state reaches two million cases
California’s health care system is buckling under the strain of the nation’s largest coronavirus outbreak and authorities say it may fracture in weeks if people ignore holiday social distancing
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.California s health care system is buckling under the strain of the nation's largest coronavirus outbreak and may fracture in weeks if people ignore holiday social distancing, health officials warned as the number of people needing beds and specialized care soared to previously unimagined levels.
Top executives from the state’s largest hospital systems —Kaiser Permanente, Dignity Health and Sutter Health, which together cover 15 million Californians — said Tuesday that increasingly exhausted staff, many pressed into service outside their normal duties, are now attending to COVID-19 patients stacked up in hallways and conference rooms.
The CEO of the Martin Luther King, Jr. Community Hospital in Los Angeles Dr. Elaine Batchlor, separately said patients there have spilled over into the gift shop and five tents outside the emergency department.
“We don’t have space for anybody. We’ve been holding patients for days because we can’t get them transferred, can’t get beds for them,” said Dr. Alexis Lenz, an emergency room physician at El Centro Regional Medical Center in Imperial County, in the southeast corner of the state. The facility has erected a 50-bed tent in its parking lot and was converting three operating rooms to virus care.
California is closing in on 2 million confirmed cases of COVID-19. The state on Tuesday reported nearly 32,700 newly confirmed cases. Another 653 patients were admitted to hospitals — one of the biggest one-day hospitalization jumps — for a total approaching 18,000.
State data models have predicted the hospitalizations could top 100,000 in a month if current rates continue.
Even more worrying than lack of beds is a lack of personnel. The pool of available travel nurses is drying up as demand for them jumped 44% over the last month, with California, Texas, Florida, New York and Minnesota requesting the most extra staff, according to San Diego-based health care staffing firm Aya Healthcare.
“We’re now in a situation where we have surges all across the country, so nobody has many nurses to spare,” said Dr. Janet Coffman, a professor of public policy at the University of California in San Francisco.
California is reaching out to places like Australia and Taiwan to fill the need for 3,000 temporary medical workers, particularly nurses trained in critical care.
Around the country, outbreaks are being blamed on lack of social distancing and mask-wearing during Thanksgiving and officials fear an even worse surge if people gather for Christmas and New Year’s.
Fresno County in California's agricultural Central Valley is in desperate condition. Dr. Thomas Utecht, chief medical officer for Community Medical Centers Fresno, related how medical staff daily see sobbing families, desperate patients and people dying in isolation wards with their loved ones watching remotely.
Doctors and health officials there are begging people to avoid gathering outside of their immediate families.
“If people don’t stay home ... we’re going to see something that’s, it’s hard for me to even imagine,” said Dr. Patrick Macmillan, palliative specialist in Fresno County. “I think it will break the health care system.”
Similar warnings echoed around the country, from Tennessee, which is seeing the nation’s worst new COVID-19 infection surge per capita, to Mississippi and West Virginia, which surpassed their previous highs for virus deaths reported in a single day on Tuesday.
COVID-19's impact isn't just on the infected. Lack of beds or nurses means that there are long lines to emergency rooms for other patients as well, such as those with heart attacks or trauma, and paramedics who must wait for an ER nurse to take charge of a patient may not be able to immediately answer another 911 call, said Dr. Anneli von Reinhart, an emergency physician at Community Regional Medical Center in downtown Fresno.
In the midst of the surge, the distribution of thousands of doses of COVID-19 vaccine to health care workers does mark light at the end of the tunnel but “it also feels like the tunnel is narrowing," said Dr. Rais Vohra, interim health officer for Fresno County.
“It’s just a race against time to try to get people through this tunnel as safely as possible,” he said. “That’s exactly what it feels like to be working on the front lines right now.”
___
Thompson reported from Sacramento, California. Associated Press reporters from around the U.S. contributed to this report.