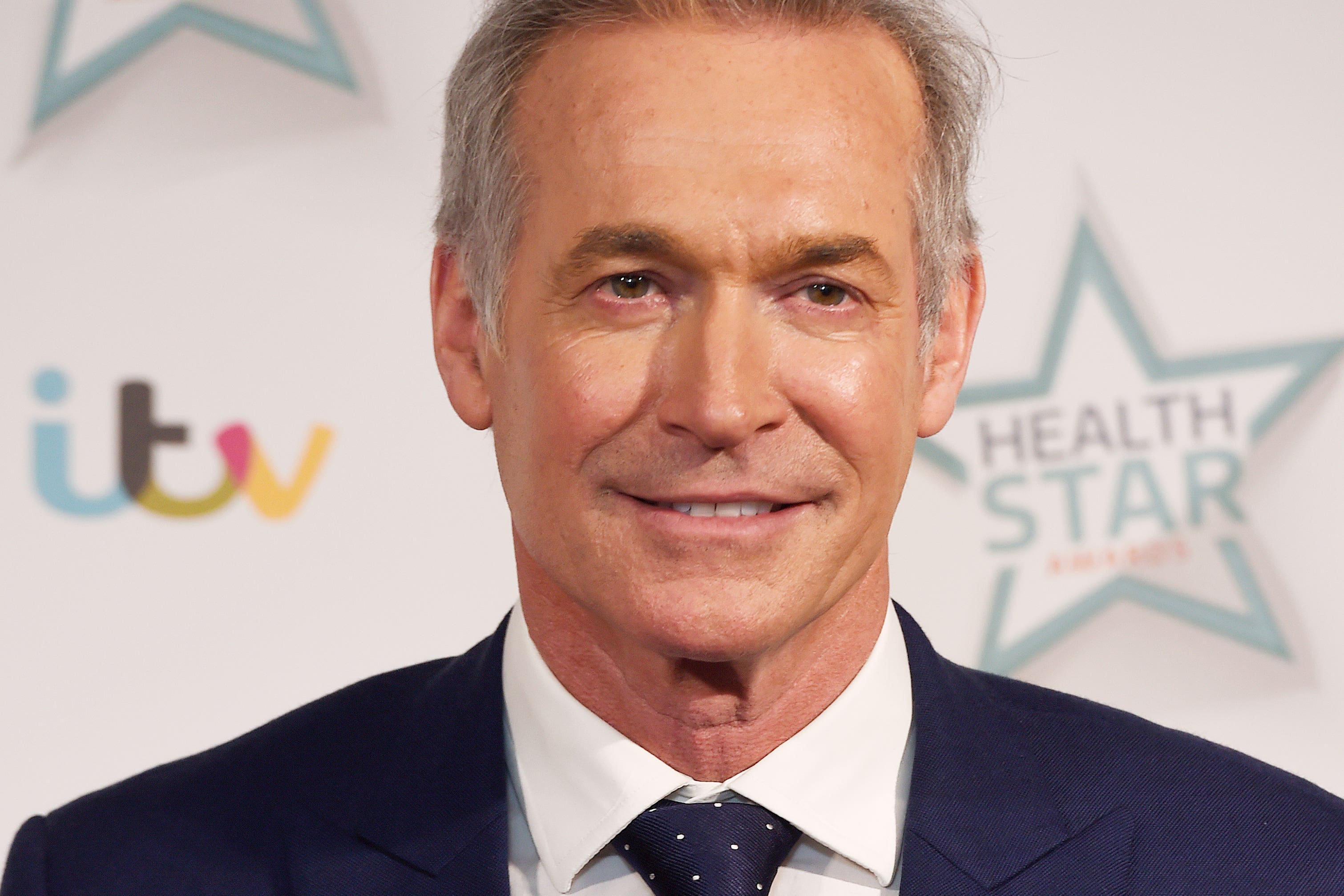
TV doctor Hilary Jones blasts Government over ‘at risk of collapse’ NHS
The GP said the health service is in crisis and warned it could be ‘finished’ if ministers do not act.
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.TV presenter Dr Hilary Jones has blasted the Prime Minister over his handling of the NHS, warning it is at risk of collapse.
Speaking on ITV’s Good Morning Britain, the GP shared the experiences of “heartbroken” frontline doctors and said if the situation “doesn’t change very quickly, the NHS is finished”.
He referred to a group chat between 13,000 doctors who work on the front line and in primary care, saying: “There are thousands of these posts and I’ve just picked three of them here as examples and they are very worrying.
“(The first one is) ‘In our hospital, we have such a long wait to get into the acute medical unit that we have a junior doctor on the roster called the ‘car triage’. This means they spend their whole shift checking on people waiting outside in their cars’.”
I've never known the NHS in such a bad situation. And if it doesn't change very quickly, the NHS is finished. It's not sustainable, it's going to collapse
“The second one – new terms that this doctor has learned this week – are reverse boarding. ‘(This) is the term used to explain the process of kicking a patient out of a recessed cubicle space in emergency care and placing them in a corridor so that a more critical patient can take their place. We did this so a patient could die anywhere other than in the corridor’.”
Dr Jones said a third message came from a doctor who said that twice this month they have had patients “miss the window” for thrombosis stroke treatment “because they’d been sat in an ambulance in our hospital car park for too long. That’s two people with life-changing disabilities that could have been prevented. I am heartbroken.”
Dr Jones described how staff are in tears at the end of their shift “and when they return to the next shift, the same patient is still waiting to be seen after 24 hours”.
He added: “For Rishi Sunak and the Government to pretend that this is not a crisis when more than a dozen trusts have announced critical incidents is not only delusional, as the BMA say, I would say at the very best it’s ill-informed misjudgment, at the very worst it’s total irresponsibility and incompetence. I have never known anything like this.”
Asked what he would say to Mr Sunak, he said: “My first statement would be that maths is certainly important to the Prime Minister because one, two, three, four, five, six, seven million people are on NHS waiting lists today, and it’s only going to get worse.
“What is he going to do about this? If this isn’t a crisis, what is?
“I’ve never known the NHS in such a bad situation. And if it doesn’t change very quickly, the NHS is finished. It’s not sustainable, it’s going to collapse.
“And that means that the very worst off people, the sickest people, will not get the care that we have become used to in the last few decades.”
It comes after the Health Secretary appeared to blame high numbers of flu cases, Covid-19 and Strep A fears for the particular pressures the NHS faced over Christmas – a claim refuted by some health experts.
Steve Barclay told broadcasters on Tuesday: “There’s £500 million of investment this year going into tackling the pressure in terms of social care.
“So we’re putting more funding in. We’ve got more clinicians, we’ve got more staff working in the NHS.
“Of course there’s a range of factors that we need to do. There’s been particular pressures over Christmas because we’ve had a surge in flu cases, Covid cases and also a lot of concern around Strep A.”
In comments to the PA news agency on Tuesday, Dr Adrian Boyle, president of the Royal College of Emergency Medicine, said it is “disingenuous to blame the current situation on the pandemic”.
He added: “It is beyond doubt that Covid made a bad situation worse but the structural problems were there long before.
“Emergency care performance has been deteriorating for nearly a decade, which is a consequence of wider staffing issues within the NHS, lack of beds and capacity, and lack of social care – all problems which are due to under-resourcing.”
Dr Tim Cooksley, president of the Society for Acute Medicine, told PA: “Whilst the twindemic of flu and Covid-19 are contributors, the fundamental problem remains a significant shortage of workforce leading to woefully inadequate inpatient bed and social care capacity. Current levels of staff burn-out and poor morale markedly exacerbate this issue.”
Matthew Taylor, chief executive of the NHS Confederation, said in a statement to PA that the Government “must do all it can to support the NHS at this time”.
He added: “We already went into the pandemic with far too many vacancies – they now stand at over 130,000 – and we were coming off the back of the longest financial squeeze in the NHS’s history.”
He added: “All of this meant the NHS wasn’t match-fit for Covid and services continue to struggle against the widening gap between demand for care and the capacity we have in the NHS.”
Shadow health minister Dr Rosena Allin-Khan said on Wednesday that she has been an emergency doctor for 17 years and “this is the worst I have ever seen our NHS”.
“People are being treated in the most undignified of ways,” she said.
Louise Ansari, national director for Healthwatch England, said: “While we know the NHS is still providing vital treatment to the vast majority of those in need, it is also clear to us that the experience of accessing care is getting worse and that, tragically, for some people they are not getting the help they need in time.”
The Doctors’ Association UK said it has written an open letter to Mr Sunak and shared doctor stories, including of a patient who could have survived with quicker care.
The medic said of the patient: “He’d been in the waiting room for eight hours before collapsing and being moved to resus. If the waiting time had been less, and he’d been seen a few hours sooner he’d have probably survived.”
A GP in Manchester also told of having to take patients to A&E owing to long waits for ambulances, including one patient with sepsis and another at risk of cardiac arrest.