Blood test that can rapidly identify sepsis being trialled in UK
The non-invasive and inexpensive test is being trialled for the first time in UK hospitals.
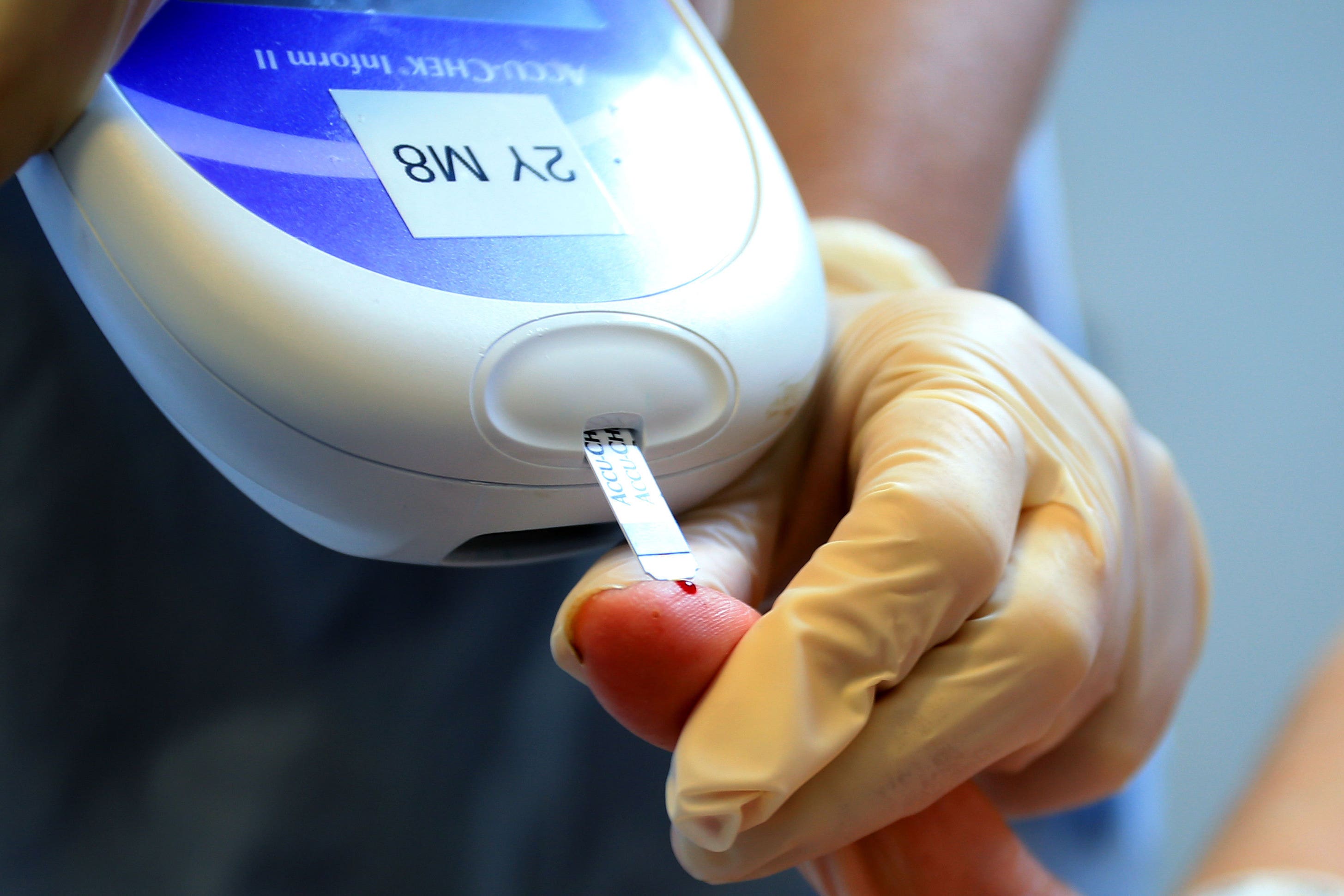
A blood test that can rapidly identify sepsis in patients has been developed and could provide a breakthrough in treating a condition difficult to diagnose.
The non-invasive and inexpensive test, which uses patient blood samples to identify high levels of DNA fragments associated with the condition in just 45 minutes, is being trialled for the first time at two UK hospitals.
If successful in a wider trial, it could be used to screen patients for the illness when they present with symptoms at A&E or if their condition deteriorates on a hospital ward.
It could also help doctors identify the sickest patients quicker and respond faster to prevent someone rapidly becoming more ill.
Sepsis, also known as blood poisoning, is difficult to identify and there is currently no test to diagnose it.
Detecting sepsis early is critical to saving lives. Sepsis is the number one cause of death in hospitals and mortality increases as much as 8% for every hour that treatment is delayed
Without prompt treatment, the condition can lead to multiple organ failure and death.
Every year in the UK there are 48,000 sepsis-related deaths, according to the UK Sepsis Trust.
Early results suggest the test, which is being trialled at Guy’s and St Thomas’ hospitals in London, can identify patients who may be at higher risk of developing sepsis and progressing to organ failure.
It works by identifying a protein found in neutrophil extracellular traps (NETs), a spider-like web of DNA released by the immune system when it goes into overdrive, which cause sepsis.
Quantifying the levels of these proteins in the blood will indicate if someone has too many NETs and is therefore is more likely to have or develop sepsis.
This is the first time a test to detect NETs directly has been brought to the bedside.
The year-long study, launched on November 27 with funding from Volition Diagnostics UK, will test the protein levels of 500 people with sepsis or septic shock in the intensive care unit at St Thomas’ hospital.
Any test which can help us to identify which patients are at increased risk of sepsis can ensure that we identify and treat patients with the most urgent need first: if this research demonstrates that NET proteins fulfil their promise as a risk stratification tool then lives will undoubtedly be saved
No additional blood samples are required from participants and the success of the new test will be compared with the existing standard blood tests used by clinicians to evaluate sepsis, which cannot diagnose the condition in isolation.
If proven to work, the new test could also help doctors triage patients, making it easier to plan admissions and discharge from critical care.
There is ongoing research into the role of NETs as a potential new treatment for sepsis.
Dr Andrew Retter, critical care consultant at Guy’s and St Thomas’, who is leading the study, said: “Detecting sepsis early is critical to saving lives. Sepsis is the number one cause of death in hospitals and mortality increases as much as 8% for every hour that treatment is delayed.
“Being able to spot those patients most at risk of sepsis using a simple blood test would be a paradigm shift in the field and could save thousands of lives every year.”
Dr Ron Daniels BEM, founder and joint chief executive of the UK Sepsis Trust, said: “Sepsis is one of the biggest causes of avoidable harm and death within our NHS.
“Delays in diagnosis result not only in lives lost, and not only in increased cost of care, but also in poor outcomes for survivors, including disability.
“Any test which can help us to identify which patients are at increased risk of sepsis can ensure that we identify and treat patients with the most urgent need first: if this research demonstrates that NET proteins fulfil their promise as a risk stratification tool then lives will undoubtedly be saved.”
Bookmark popover
Removed from bookmarks