Foetal science research: Providing a lifeline in the womb
If this new treatment works, it could open the door to curing a variety of hereditary disorders before birth

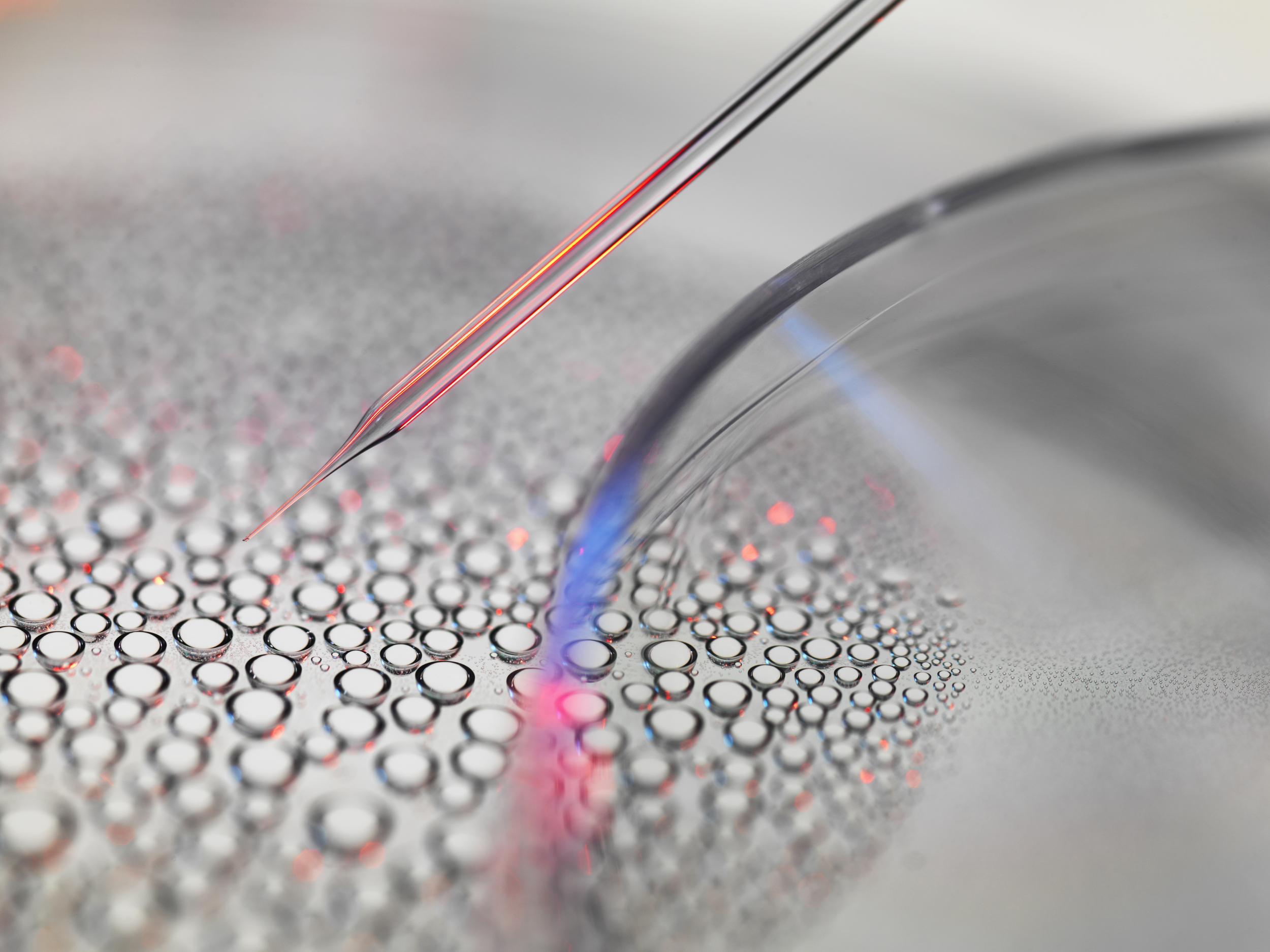
In the three months before she was born, Elianna Constantino received five blood transfusions and a bone-marrow transplant. All were given with a needle passed through her mother’s abdomen and uterus, into the vein in her umbilical cord.
Elianna, born 1 February with a robust cry and a cap of gleaming black hair, has a genetic disease that usually kills a foetus before birth. The condition, alpha thalassaemia major, leaves red blood cells unable to carry oxygen around the body, causing severe anaemia, heart failure and brain damage.
The transfusions in the womb kept her alive, but only treated her illness. The bone-marrow transplant has the potential to cure it. Whether it will succeed is still too soon to tell.
Elianna and her mother, Nichelle Obar, were the first patients in an experiment that pushes the limits of foetal therapy, a field already known for its daring approach.
If the treatment works, it could open the door to using bone-marrow transplants before birth to cure not just Elianna’s blood disease but also sickle cell anaemia, haemophilia and other hereditary disorders, some so severe that the prenatal diagnosis may lead parents to end the pregnancy.
Bone marrow is considered a potential cure because it teems with stem cells, which can create replacements for cells that are missing or defective as a result of genetic flaws.
“This line of work moves the field of foetal surgery, which currently consists of big operations for anatomic disorders, in a new direction of molecular and cellular therapies given non-invasively,” says Dr Tippi MacKenzie, a paediatric and foetal surgeon who is leading the study at the UCSF Benioff Children’s Hospital in San Francisco.
Obar, 40, and her husband Chris Constantino, 37, are healthy but learned during her first pregnancy that they are thalassaemia carriers. There are several forms of the disease, and worldwide about 100,000 children a year are born with severe cases. Millions of people are carriers, most commonly those from Asia, the Mediterranean, Africa or the Middle East.
Carriers are generally healthy, but when two have children together, the children are at risk of being born with the disease. Obar’s ancestry is Filipino and Puerto Rican; her husband’s is Filipino. They live in Kilauea, on the Hawaiian island of Kauai.
Their first child, Gabriel, now three, is healthy. But each child they conceive has a one in four chance of being affected, and during Obar’s second pregnancy, her doctors were on the lookout for the disease.
They found it. An ultrasound at 18 weeks showed that Elianna’s heart was twice the size it should have been, and fluid was accumulating around her lungs and other organs. Blood flow through her brain was abnormally rapid, a sign of severe anaemia.
Everything pointed towards alpha thalassaemia major – the most severe form of the disease. Obar’s doctor and genetic counsellor warned her and her husband that their daughter might not survive.
“Her heart was working so hard,” Obar says, with tears in her eyes.
By this point in pregnancy, the second trimester, an affected foetus has little or no working haemoglobin, the molecule that carries oxygen to cells all over the body. Tissues are suffocating, and the heart struggles to compensate.
Some medical references describe the illness as “incompatible with life”, and most foetuses die in the womb from heart failure. The pregnancy may end in miscarriage, and parents may not know why. Many do not know they are carriers.
Sometimes, as the foetus weakens, a phenomenon called mirror syndrome occurs: the mother also becomes ill, with severe high blood pressure and other problems that can kill her unless the pregnancy is ended.
Infants with untreated alpha thalassaemia major who somehow survive until birth almost always have severe brain damage from lack of oxygen.
Transfusions into the umbilical cord during pregnancy can save the foetus and may prevent brain damage. The child will then require transfusions every three or four weeks for life; the procedures cost about $50,000 (£37,600) a year and pose their own risks, especially a dangerous buildup of iron.
A bone-marrow transplant after birth can cure the disease, but only if a matching donor is found. The transplant also has dangers, and costs about $150,000.

Many obstetricians do not even tell patients about transfusions, MacKenzie says.
“Everyone now is told to abort,” says Dr Elliott Vichinsky, one of MacKenzie’s research partners and the founder of the Northern California Comprehensive Thalassaemia Centre at the UCSF Benioff Children’s Hospital Oakland. “We understand families should make that decision if that’s right for them. We’re just saying they should be given the information that there are other options.”
Some doctors are wary of transfusions because they think that even if the child survives, there is still too high a risk of significant brain damage. A report last year on an international registry of survivors found that 20 per cent (11 of 55) had serious delays in their neurological development. Another article found delays in 29 percent (4 of 14).
MacKenzie and Vichinsky say they did not try to discourage parents who preferred abortion. But some parents would rather avoid it.
“These are not unwanted pregnancies,” MacKenzie says. “We’re as pro-choice as you get. These are wanted pregnancies for whom therapy could be offered. And you can have a choice to terminate or you can have a choice to have therapy, but the bottom line is you have to be given those choices. And we recognise that’s a very personal choice, but we as doctors need to be providing you with those choices.”
Obar’s genetic counsellor mentioned termination – but also transfusions. She and her husband chose transfusions.
The counsellor also described MacKenzie’s study. The chance that the transplant might help their daughter appealed to them, though they understood that it was an experiment and that there were no guarantees. At this early stage in the research, the primary aim of the study was to find out whether the treatment was safe.
The general goal of foetal therapy is to act early enough to minimise or even prevent lasting harm from severe problems that start in the womb. With a bone-marrow transplant, the added advantage of giving it before birth is that the foetal immune system is not yet fully developed, so it is unlikely to reject the transplant.
In contrast, when transplants are given after birth, the child first needs an arduous course of chemotherapy to wipe out the immune system and prevent rejection. That treatment itself can be fatal: the death rate is about 7 per cent, mostly from infection.
Bone-marrow transplants in foetuses, sometimes using the father as a donor, were first tried in the 1990s. Some worked, but most failed, and doctors mostly abandoned the procedure, MacKenzie says.

But research continued in animals, and a key finding emerged: the mother, not the foetus, was rejecting transplants that came from fathers or other donors.
A possible solution became evident. “Everybody has a perfect donor when they’re a foetus, and that’s the mom,” MacKenzie says.
Genetically, the mother is not a complete match – half the foetal genes come from the father – but she’s still the ideal donor before birth, because during pregnancy the maternal and foetal immune systems are at peace. Mother and child tolerate one another: their cells do not fight. The truce ends at birth, or shortly before, when the infant’s immune system starts to work.
It may seem puzzling to give a foetus with a genetic disease stem cells from the mother who passed on the bad genes. But it can work. If the mother is a healthy carrier, her stem cells also have copies of the good genes that the child needs.
People have two copies of nearly every gene; one copy from each parent. Alpha thalassaemia major involves two genes, and two flawed copies of each.
A foetus with the disorder has four bad copies. But each parent has only two bad copies – and two good ones. So the mother’s stem cells can produce healthy blood cells for the child.
On Obar’s first visit to UCSF in October, at 21 weeks of pregnancy, Elianna was so sick that the team feared she was near death, and gave her a transfusion almost immediately, MacKenzie says. She quickly began to improve.
The team then drew bone marrow from Obar’s hip bones, and along with Elianna’s second transfusion – about a week after the first – they dripped in about 50 million of her mother’s stem cells, an enormous number compared with usual transplants.
Stem cells home in on the bone marrow, and the reason for such a big dose was to give the new cells the best possible chance to displace Elianna’s defective ones and produce a healthy blood supply for her. She had three more transfusions over the next few months, until her birth.
In one sense, the experiment has already been a success: there have been no adverse effects to mother or baby, so the treatment seems safe.
“I’m thrilled that it was safe and it was feasible,” MacKenzie says, adding it was also important “to get the message out that foetal transfusions for alpha thalassaemia are lifesaving”. She expects to perform transplants on a few more patients, see how they fare and then decide how to proceed.
So far for Elianna, in her first three months, there has been no obvious benefit from the transplant. Like all children with her blood disorder, she needs a transfusion every three weeks.
But tests have found some of her mother’s stem cells in her blood. Whether they will start to help her is unknown. If they do not, her parents could eventually opt for a bone-marrow transplant to cure the disease and free her from a lifetime of transfusions.
© New York Times
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks