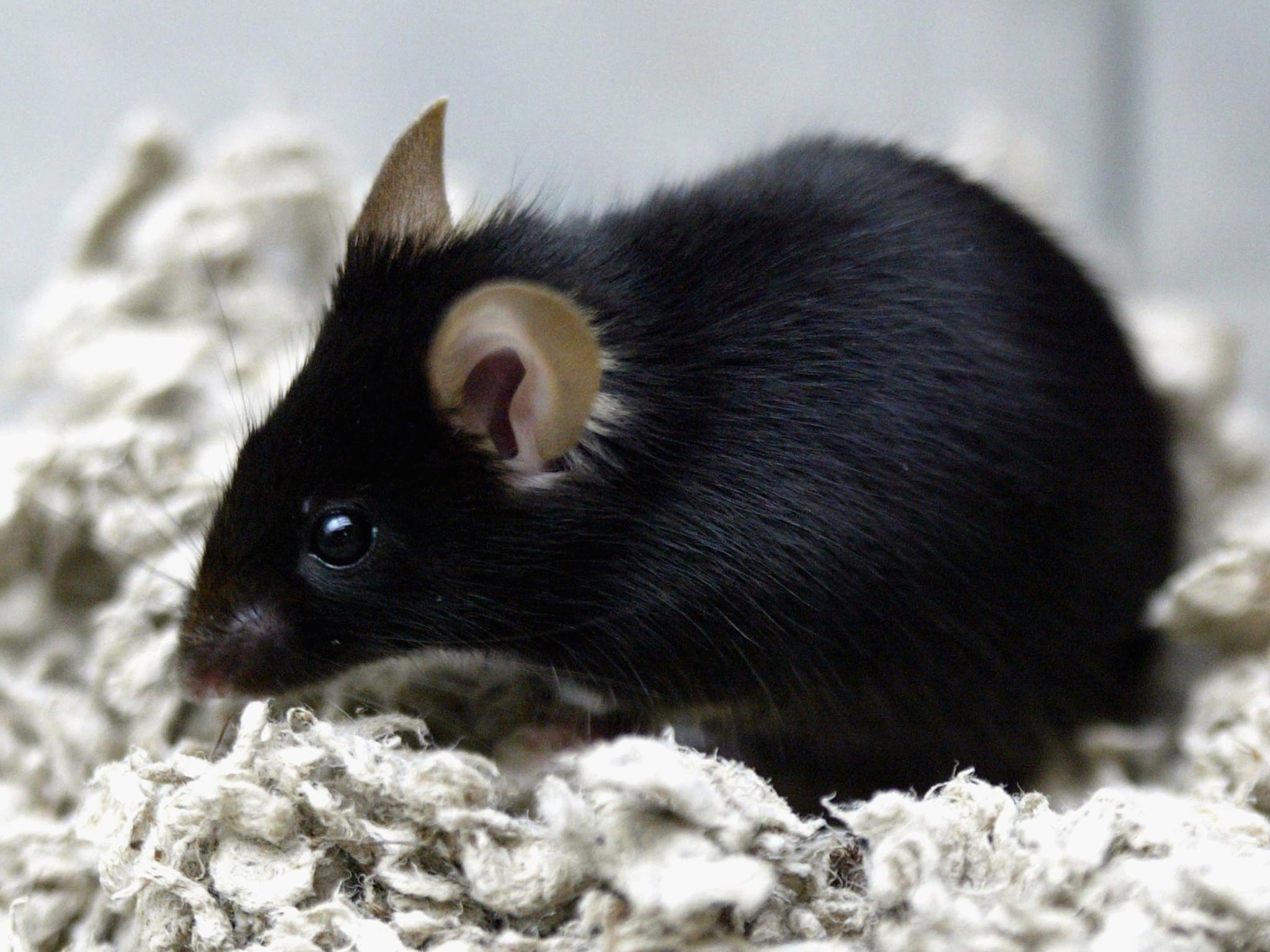
Diet pill that makes you feel full proven to keep weight off in mice, scientists say
New drug fexaramine has fewer side-effects than other pharmaceuticals

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A pill that makes you feel as if you have just eaten an imaginary meal has prevented weight gain, lowered cholesterol and controlled levels of sugar in the blood – at least in laboratory mice, a study has found.
The inventors of the drug said that unlike similar dietary pills it is designed to stay within the intestines and not to circulate in the bloodstream, making it inherently safer with fewer side-effects than other pharmaceuticals aimed at preventing obesity.
Clinical trials on humans are planned, the scientists said. It will become the latest in a number of prototype drugs aimed at combating the obesity crisis through appetite suppression, feelings of satiety or other ways of curbing calorie intake.
“This pill is like an imaginary meal. It sends out the same signals that normally happen when you eat a lot of food, so that the body starts clearing out space to store it. But there are no calories and no change in appetite,” said Ronald Evans of the Salk Institute in La Jolla, California.
The drug, called fexaramine, targets a protein on the surface of the cells in the digestive system called the farensoid X receptor (FXR), which triggers the release of bile acids from the liver in preparation for the digestion of food, as well as being involved in the storage of fats and sugars.
Normally, the FXR receptor is turned on at the beginning of a meal in anticipation of there being an influx of food and calories. It also induces changes to blood sugar levels and causes the body to burn some fats before a meal, Dr Evans said.
Other drugs can also turn on the FXR receptor in the intestines but they also work in the liver, kidneys and adrenal glands. However, the fexaramine pill developed by the Salk researchers stays within the intestine and targets only the cells of the gut, they said.
“When you eat, you have to quickly activate a series of responses all throughout the body and the reality is that the very first responder for all this is the intestine,” Dr Evans said.
When the scientists fed the drug to obese mice for five weeks they stopped putting on weight, lost fat and had lower blood sugar and cholesterol levels compared with untreated mice.
The study, published in Nature Medicine, also found that the mice had raised body temperatures, which indicates that their metabolism had increased, and that some of their white fat deposits – associated with ill health – were converted to less-damaging brown fat.
A crucial observation was that the fexaramine, when given orally, stays within the intestines and as a result appears to work better than other drugs aimed at stimulating the FXR receptor that enter the bloodstream, Dr Evans said.
This means that the drug follows the “natural order” of how the FXR is normally turned on, by activating the cells of the gut before other parts of the digestive system, he said.
“The body’s response to a meal is like a relay race, and if you tell all the runners to go at the same time, you’ll never pass on the baton. We’ve learned how to trigger the first runner so that the rest of the events happen in a natural order,” Dr Evans said.
Nick Finer of University College London, who was not involved in the research, said that the Salk study has shown that fexaramine mimics how bile acids interact with gut receptors, reduces weight gain and increases energy expenditure by converting ordinary white fat into brown fat, a tissue what can generate heat.
“These findings are potentially of great importance to our basic understanding of how energy intake is balanced by energy expenditure and, potentially, as to why this system is mismatched in those who gain – or lose – excessive weight,” Professor Finer said.
“In the long-term it also offers a new approach to potential treatment of human obesity. Mice however are not human and much work is still needed to see if the effects of fexaramine are the same in humans and to establish its safety,” he said.
Other scientists are also working on ways of converting “bad” fat into “good” brown fat, while some researchers have combined a fatty acid called propionate with a form of a dietary fibre inulin which when eaten generates the release of appetite-suppression hormones from the gut wall.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments