The ‘possibilities are endless’ – or are they? The evolutionary journey that Covid could take
Some see an infinite capacity for the virus to evolve, others believe it has a genetic endpoint. It’s an issue that will shape our fight against Covid-19, as science correspondent Samuel Lovett explains

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Imagine the scenario. Covid case rates are once again soaring in a poorly vaccinated population within eastern Africa. The rollout of jabs has been slow, hampered by inconsistent supplies. Due to limited testing capacity, officials are unsure of the true scale of the country’s growing wave, but the pressure on hospitals is undeniable. Intensive care units are filling up. Nurses and doctors are overwhelmed. Covid-19 is rife.
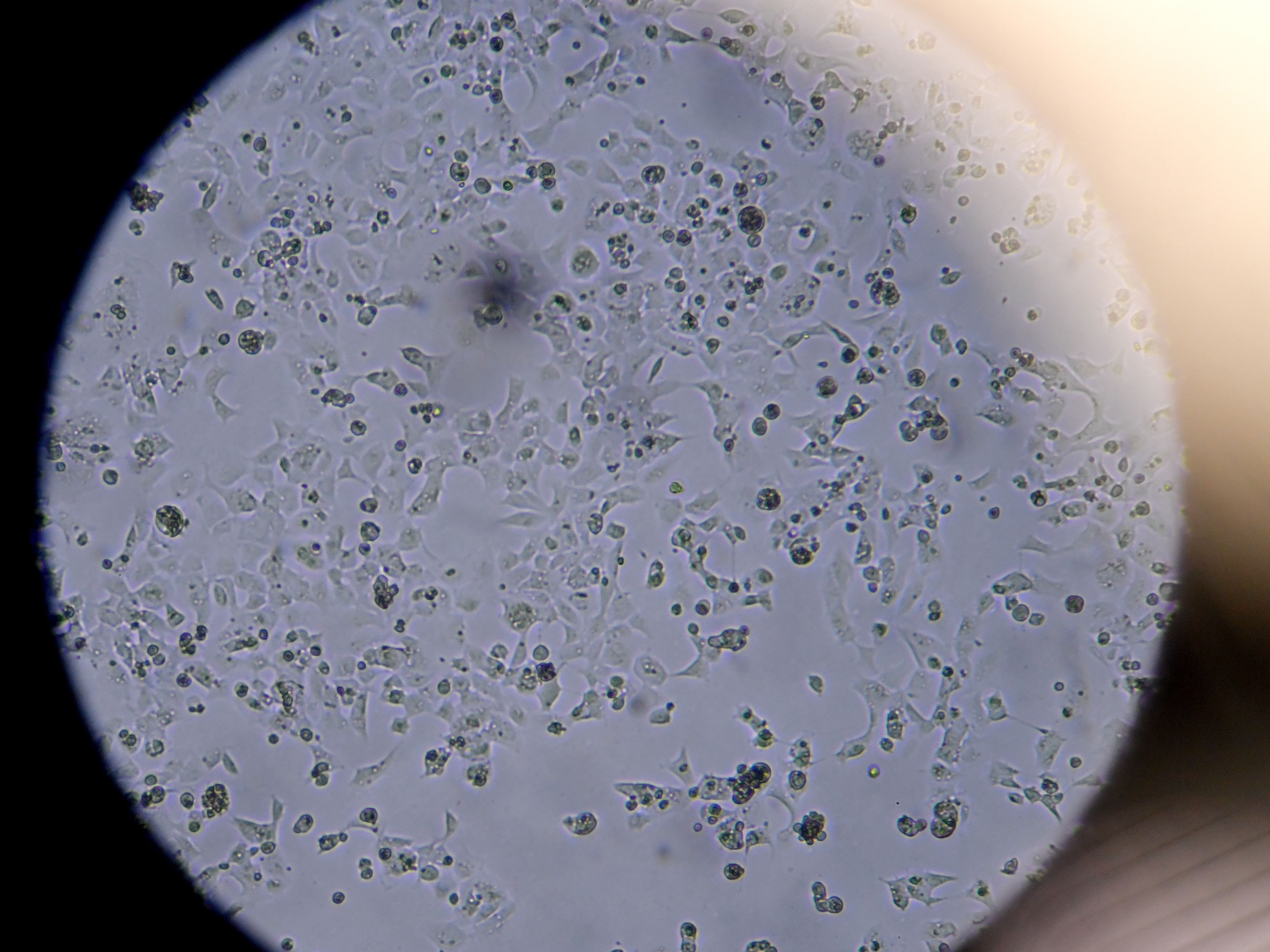
In one of the hospitals, an immunocompromised patient is infected. The virus buries itself deep in the individual, who struggles to clear the infection. Three months pass, yet the patient is continuing to test positive. During that time, the virus has been replicating, mutating, acquiring new characteristics and improving its fitness.
A vaccinated nurse is the next victim. He doesn’t display any obvious symptoms, so is unaware of the infection, but the rest of his family haven’t been jabbed. It takes a whole week after the initial exposure for them to fall ill, by which the point the virus has been passed on to many others in the local area. Highly transmissible, immune-evading and more pathogenic than previous variants, the newly-mutated virus kick-starts a new wave of infections throughout the country and beyond.
This development of events is not beyond the realm of possibility. As those in the West build up their walls of immunity, persistently high infection rates and stuttering vaccine programmes in the Global South threaten to give rise to a new Covid variant – one that could bring many parts of the world back to square one.
Globally, daily infections are approaching the 700,000 mark. A caseload of this size means billions and billions of copies of the virus are replicating within our cells each day – ample opportunity, or “wriggle room”, as virologist Dr Stephen Griffin puts it, for dangerous variants to emerge.
The conditions are certainly ripe for the continued evolution of the Covid virus, but how much further can it realistically go? Sars-CoV-2 remains a relatively new human pathogen, so will still be adjusting to our bodies, but there is uncertainty whether this process of adaption can last forever.
There are two (loose) schools of thought: those that see an infinite capacity for the virus to evolve, and those who believe there is a genetic endpoint. “There is a very large amount of evolutionary landscape that the virus can explore,” says Jonathan Ball, a virologist at Nottingham University. But, he says, that doesn’t necessarily mean the virus will venture into this space.
The vast majority of mutations that have been recorded to date are concentrated in the Sars-CoV-2 spike protein – the part of the virus responsible for binding to human cells and gaining entry. Our immune system, as trained by natural infection or vaccination, targets these structures to block future infection and prevent illness.
But through random mutations that crop up during replication, some of which confer an advantage to Sars-CoV-2 and are retained by future viral copies, the shape of this spike protein can change to evade our immunological defences and improve the efficiency with which it binds to human cells. As a result, seemingly protected people may be susceptible to reinfection – an event that has been associated with the Delta variant.
With time, Sars-CoV-2 has accumulated a constellation of mutations in the spike protein through the process of antigenic drift. “These changes happen usually one by one, or certainly in small numbers,” says Professor Ball. “So you don’t suddenly get a huge genetic change in a single virus.”
Each mutation gradually takes the virus further away from the original version that emerged in Wuhan. Some will steer the pathogen down a genetic cul-de-sac, while others will strengthen it, culminating in the emergence of problematic variants such as Alpha, Beta and Delta.
But in the context of the spike protein, “the virus will have constraints,” argues Emma Thomson, a professor in infectious diseases at Glasgow University’s Centre for Virus Research. Across the world, the same changes – such as the infamous E484K mutation, nicknamed “Eek” by some scientists – have been emerging independent of one another.
Known as convergent evolution, this suggests there is a set pathway for the virus to journey down. Any mutation that arises outside of these parameters is likely to be ineffective in improving the ability of Sars-CoV-2 to bind with our cells or evade our antibodies.
“We’ve seen the same mutations in Brazil and South Africa, and India to some extent,” says Professor Danny Altmann, an immunologist at Imperial College London. “There’s rather limited positions which the virus can move into. It can’t transform itself forever.”
In essence, the virus is coming up with the same solutions to the same problems. For now, at least, it’s continuing to lose out against our immune system – but should it eventually stumble upon a winning combination of mutations within that pathway, there’s likely to be trouble.
For Aris Katzourakis, a professor of evolution and genomics at the University of Oxford, the “possibilities are endless”. He suggests the genetic pathway may be wider than we realise, and believes that it could be broadened if certain mutations buried deep in the virus’ coding are eventually accessed through antigenic drift.
“Even if there are limits, there’s always some change somewhere else that might unlock possibilities that were previously not seen,” he says. “E484K, for example, that mutation itself might unlock a whole load of other mutations elsewhere in the spike that we’re going to see in the next six to 12 months.”
The spike may be the main point of focus for now, but scientists believe there are other areas of Sars-CoV-2 which could be susceptible to mutations that improve the fitness of the virus. With an exceptionally large genome, which codes for the formation of many different proteins, there is plenty of scope for variation in other domains of the pathogen.
“There are changes that can occur anywhere in the genome which affect how the virus behaves,” says Professor Ball. Some mutations could improve the efficiency of the virus’ ability to replicate once it’s gained entry to our cells, he adds. This could heighten the viral load generated by a particular variant, making it harder to clear the infection – even in a vaccinated individual.
The “magnitude” of replication could also allow the virus to “spread faster around the body and be better at outrunning immune responses”, says Dr Griffin. This could lead to different timescales of disease, or even make the virus more pathogenic, he adds.
Another option available to the virus is the far more sudden and abrupt process of recombination. These events occur when two variants infect the same host and swap parts of their genome during viral replication, like a pack of cards being reshuffled and dealt out.
In the early days of the pandemic, due to the limited genetic diversity of Sars-CoV-2, recombination was seen as largely inconsequential, with similar-looking variants exchanging much of the same genetic coding – or cards – between each other.
But as the virus continues to spread – particularly in countries where it is given free rein to do so – it will build up genetic diversity that could make recombination more pronounced, and produce an offspring variant that holds the right hand needed to dominate.
“As you go forward like you do with flu, where we’ll get multiple seasons of Covid-19 stacking on top of each other, with these variants circulating, you’ll see more incidents of recombination due to individuals being infected by two or more different variants,” says Dr Julian Tang, a respiratory virologist at Leicester University.
Ultimately, the environment in which the virus is circulating cannot be forgotten in any discussion of how much further Sars-CoV-2 will continue to evolve. In a well-vaccinated population, an immune-evading variant would outcompete a highly transmissible one, driving it into extinction. Within a partially protected population, it’s likely the latter would dominate.
“It’s about two processes,” says Dr Griffin. “It’s about what you call the mutability of the genome and then it’s about how it’s interacting with its environment,” which dictates which genetic changes “set in” and “how they become established”.
A wide range of factors are at play here, including the immune response generated by vaccination and natural infection, temperature and climate, the imposition of restrictions such as social distancing or mask-wearing, racial types, and innate immunity – that line of defence which is wired to attack any foreign invader, regardless of what it looks like.
Genetic mutation and evolution may be a random process, “but it also has to match up to something,” says Dr Griffin. “That something is determined by the wider environment.”
The future of our fight against Covid comes down to whether Sars-CoV-2 will eventually evolve beyond the reach of our vaccines and the protection they provide. We now have the tools to diminish the impact of the virus, yet we cannot account for any dangerous changes that drastically alter the status quo.
The experts are confident that, under the current rules of play, we have the upper hand. But how much longer will that last?
In spite of the progress that has made over the past 18 months, along with the huge loss of life that the world has suffered, it’s still early days in the lifetime of this virus. “It normally takes many years for viruses, once they cross the species barrier, from animals to humans, to really optimise themselves to be able to replicate well,” says Professor Ball. “I wouldn’t put it past the virus to find other clever ways of evolving.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments