Report: Oversight lapses at impaired pathologist's hospital
An inspector general's report says an Arkansas veterans hospital missed the errors of a pathologist who pleaded guilty to involuntary manslaughter while working impaired due to its poor oversight
An Arkansas veterans hospital missed the errors made by a pathologist who pleaded guilty to involuntary manslaughter while working impaired due to its poor oversight, according to an inspector general's report released Wednesday.
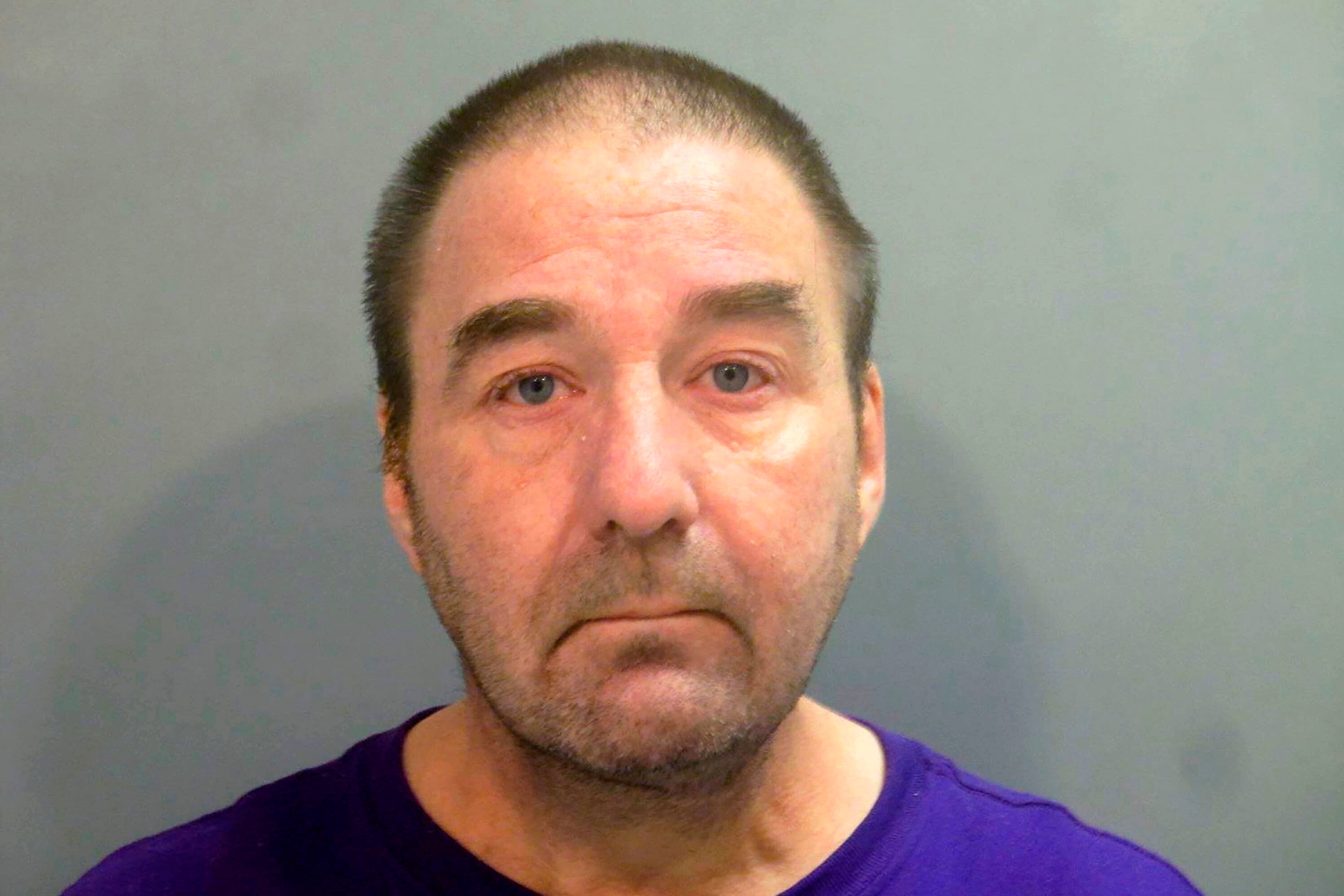
The report by the U.S. Department of Veterans Affairs inspector general criticized the Veterans Health Care System of the Ozarks where Robert Morris Levy worked, for not having a “culture of accountability" that would have encouraged others to report his mistakes without fear of reprisals.
Under an agreement with federal prosecutors, Levy pleaded guilty last year to one count of voluntary manslaughter in the death of a patient he misdiagnosed. The IG's report said lapses in the Fayetteville facility's quality management processes contributed to thousands of Levy's errors.
“Any one of these breakdowns could cause harmful results," the report said. “Occurring together and over an extended period of time, the consequences were devastating, tragic, and deadly."
Levy pleaded guilty to misdiagnosing a patient with small cell carcinoma who died after being treated for a type of cancer he didn’t have. Levy falsified the patient’s medical record to state that a second pathologist agreed with his diagnosis, according to the agreement.
Levy also pleaded guilty to one count of mail fraud for receiving 2-methyl-2-butanol, a chemical that he used to intoxicate himself but that standard drug and alcohol screenings don’t test for.
Levy was originally indicted on three counts of involuntary manslaughter in the deaths of patients prosecutors said he misdiagnosed. He was also indicted on multiple charges of fraud and making false statements for his alleged attempts to conceal his substance abuse and incorrect diagnoses.
Levy was fired from the Veterans Health Care System of the Ozarks in Fayetteville in April 2018. The hospital did not have an immediate comment on the report.
VA officials said in 2019 that outside pathologists reviewed nearly 34,000 cases handled by Levy and found more than 3,000 errors or missed diagnoses dating back to 2005. The inspector general's report said 589 of those were “major diagnostic discrepancies."
U.S. Rep. Steve Womack, whose district includes Fayetteville, said the report showed multiple failures that allowed Levy’s misconduct.
“The report details an abject failure of leadership that led to the misdiagnosis and subsequent harm to hundreds of veterans who rely on the VA health system for care,” Womack said in a statement. “It is unacceptable to limit accountability to the criminal conduct of Dr. Levy.”
The inspector general's recommendations include exploring whether to have a mandatory alcohol testing policy for employees, including healthcare workers who perform functions that would put patients at risk if they're impaired.
The report also called for the hospital to review its “psychological safety climate" to ensure patients, staff and the public feel they can report unsafe care without fear of reprisals.
Bookmark popover
Removed from bookmarks