Maryland officials failed to properly oversee prisoner health care contracts
A newly released audit says Maryland has failed to properly manage contracts with private companies that provide medical and mental health care to prisoners in state-run detention facilities
Maryland’s Department of Public Safety and Correctional Services has failed to properly manage and oversee contracts with private companies that provide medical and mental health care to prisoners in state-run detention facilities, according to a newly released audit.
The failures resulted in hundreds of missed evaluations for suicide risk and a shortage of mental health exams, among other problems. The findings stem from state auditors reviewing three contracts over roughly five years beginning in 2018.
The report cites understaffing as a potential contributing factor. It also raises questions about whether the contracts were structured in a way that benefited the companies without ensuring they provided adequate services.
Outsourcing prison medical care is becoming increasingly common across the country, but the practice often draws criticism and lawsuits alleging malpractice, neglect and substandard care.
In Maryland, the system has recently resulted in “consistent failure to provide the minimum staffing and properly complete key health examinations of incarcerated individuals,” according to the report.
Leaders with the Department of Public Safety and Correctional Services pushed back on some of the audit’s findings while largely agreeing to comply with its recommendations. Some of the issues have already been addressed under new contracts, officials said.
State officials voted earlier this year to switch prisoner health care providers, cutting ties with YesCare, which was facing significant criticism, and partnering instead with Centurion of Maryland.
The agency developed new written procedures to ensure contractors complete medical and mental health examinations within the required time, department leaders wrote.
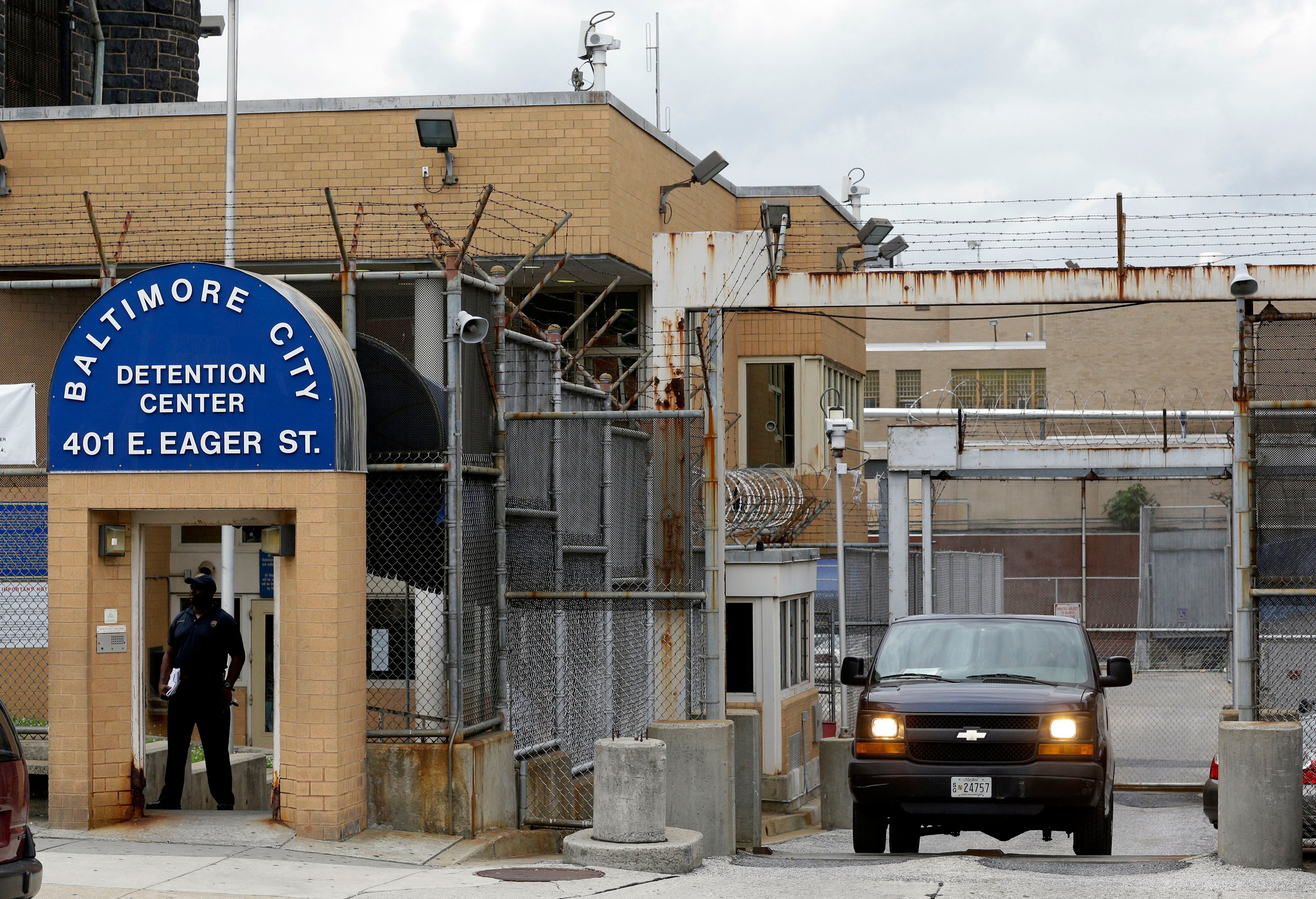
An earlier audit found vacancies across the department of over 20% in recent years and a 13% vacancy rate in June 2023. Correctional Services is responsible for thousands of incarcerated people in 18 facilities, including state prisons and Baltimore’s jail, which holds people awaiting trial.
The department’s health care costs increased significantly between 2018 and 2023 — from $120 million to $168.7 million — even as the state’s average incarcerated population declined about 18%, according to the report, which was released Tuesday by the Maryland Office of Legislative Audits.
Auditors said the corrections department was unable to justify a fixed fee structure that guaranteed companies were paid “regardless of the level of staffing provided and the actual costs incurred for equipment, supplies, and hospital visits.”
The contracts also failed to establish competitive hourly rates for medical and mental health staff, which could have contributed to recruiting and retention problems, according to the report. A registered nurse employed by the medical contractor would have been paid $25,500 less than the statewide average in 2023, auditors found.
In their written responses, corrections leaders said the new contracts include minimum wage requirements and a payment structure that incorporates fixed price incentives. Officials also agreed to ensure that all patient complaints alleging poor medical care are properly investigated.
Bookmark popover
Removed from bookmarks