How a new tuberculosis drug could stop one of the world’s deadliest diseases

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
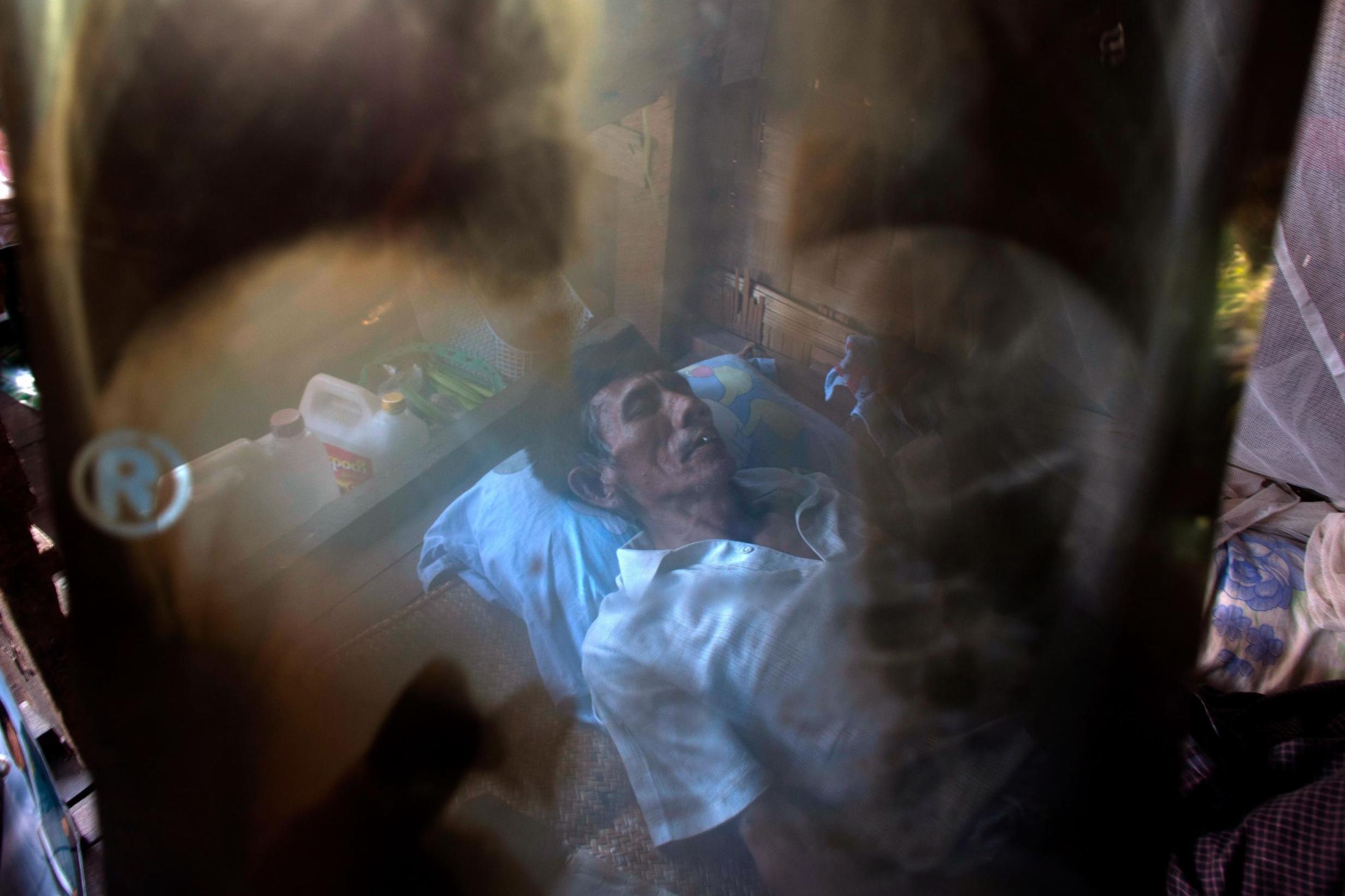
Your support makes all the difference.Tuberculosis struck 10 million people worldwide in 2017, killing 1.6 million of them – a toll greater than that of HIV, malaria, measles and Ebola combined. TB is the leading infectious killer around the globe; nearly 1.8 billion people are carrying the bacterium that causes the disease.
The world is sorely in need of new ways to prevent TB, not just treat it. Drugs to stave off the infection do exist, but the months-long regimens are difficult and people often do not finish the prescribed courses.
That may soon change. A new drug course, lasting just one month, is just as effective as longer regimens at preventing TB, scientists reported earlier this year. The results have left experts hoping for new progress against a disease that has been an intractable enemy for centuries.
“I think it’s a moment of really extraordinary promise,” says Mike Frick, co-lead for TB at Treatment Action Group, an advocacy organisation.

Among the plagues sweeping developing countries, TB has often taken a back seat to competing and urgent priorities, especially HIV. (The two are linked: HIV patients account for 1 in 5 TB deaths worldwide.)
In August, the US Food and Drug Administration approved a new drug to treat the deadliest strain of TB – but it was the first approval for a TB drug in more than 40 years. Diagnostic tests for the infection are not sensitive and mostly rely on sputum, which many sick people struggle to produce.
And prevention? “It’s really downplayed and it’s ignored, and it’s ignored to a degree that is scandalous,” says Dr Richard Chaisson, professor of medicine at Johns Hopkins University in Baltimore.
One challenge is identifying those who should receive preventive drugs. The drugs are the clear choice for the most vulnerable groups: people with HIV; people whose immune systems are compromised because they take biologic drugs for Crohn’s disease, arthritis or other diseases; and young children and others who share a home with someone infected.
Protection for these groups should last at least five years, studies suggest.
But 1 in 3 people worldwide harbour the TB bacteria, and just 1 in 10 will go on to develop the disease. Who among them should be treated?

“The biggest issue has been to identify those 10 per cent,” says Dr Eliud Wandwalo, senior coordinator for TB at the nonprofit Global Fund. “We don’t have any good indicator to show you which of these people who are infected might progress and become sick.”
For many people who are healthy, or who simply feel healthy, the drugs have been a tough sell.
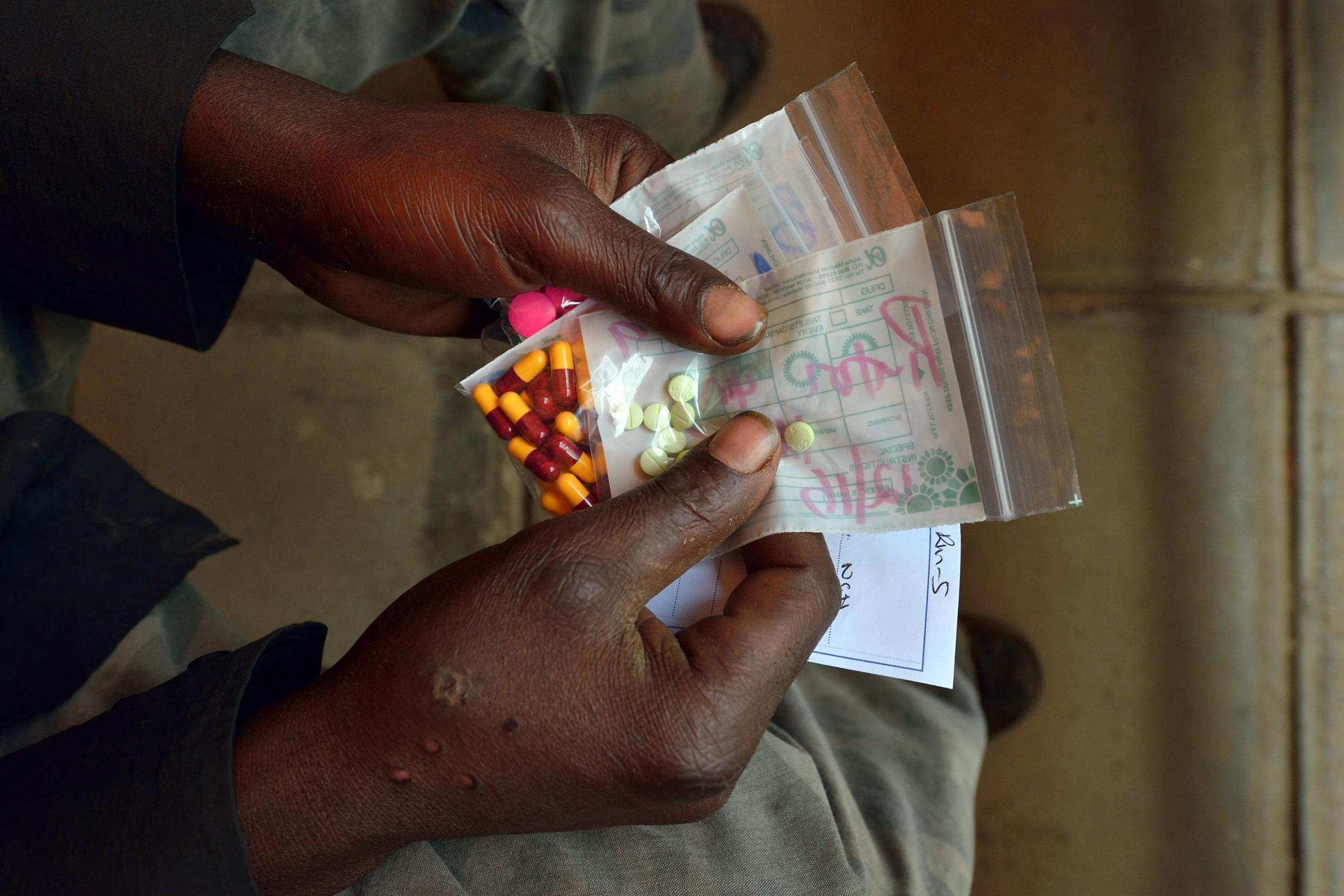
For decades, the standard course has been an antibiotic called isoniazid, which kills the bacteria causing TB only when they are replicating. The drug must be taken daily for nine months, in the hope of catching the bacteria as they multiply, and it can cause numbness, nausea and fever. Isoniazid can also cause liver toxicity, so people taking it are advised not to drink alcohol for the entire nine months.
“Traditionally, completion rates have been very poor,” says Alison Grant, an epidemiologist at the London School of Hygiene and Tropical Medicine.
Doctors sometimes decline to prescribe the antibiotic because of worries about exposing otherwise healthy people to the side effects, or contributing to a rise in drug-resistant bacteria if patients don’t complete the full course.

Both those concerns are unfounded, says Grant. Doctors “just stay away from it, despite the evidence showing otherwise”.
In the past decade, scientists have come up with two shorter courses: a drug called rifampin taken every day for four months; or a combination of isoniazid and rifapentine, taken once weekly for three months.
Still, for some people, remembering to take the pills – and all 11 pills together – once a week can be more challenging than taking them every day, says Grant.
An alternative emerged in March, when Chaisson and his colleagues published a study in the New England Journal of Medicine showing that a regimen of isoniazid and rifapentine, taken daily for one month, is as effective at preventing TB, safer and more likely to be completed than the traditional nine-month course of isoniazid.
The World Health Organisation met to review this new regimen in July and is expected to endorse it later this year. The study was conducted only in people infected with HIV, however, and it is likely that the WHO will approve the regimen only for those patients.
Chaisson thinks preventive drugs should be given to a far larger population.
“If we had an intervention for HIV that reduces mortality by 37 per cent, the WHO would have an emergency meeting and it would be recommended for uptake in the entire world,” he says. “But when it’s for TB, people just sort of shrug.”
“It’s just a stolid world of never-changing practices – slow to adopt, slow to change, slow to evolve,” Chaisson adds.
Cost is another hurdle. The one- and three-month courses both rely on rifapentine, made by Sanofi. In 2013, after a year-long advocacy campaign to lower the costs, Sanofi dropped the price of rifapentine in the three-month course from $71 (£57.50) to $32.
The new one-month course requires more rifapentine overall than the three-month regimen, and so is more expensive. Advocates and global health organisations are in intense negotiations with Sanofi to lower the cost to just $15 for the entire one-month treatment course.
At least two companies are said to be developing generic versions, which also may bring down the cost. Without a lower price, donors such as the US federal government’s President’s Emergency Plan for Aids Relief (PEPFAR) are unlikely to support the new course.
Still, experts say they are more optimistic about TB prevention than ever before.
Just a year ago, funding organisations still presented countries with a false choice between prioritising antiretroviral therapy for HIV and preventive therapy for TB, says Chaisson.
But PEPFAR has begun to prioritise TB prevention. National governments will have to follow in order to turn back TB.
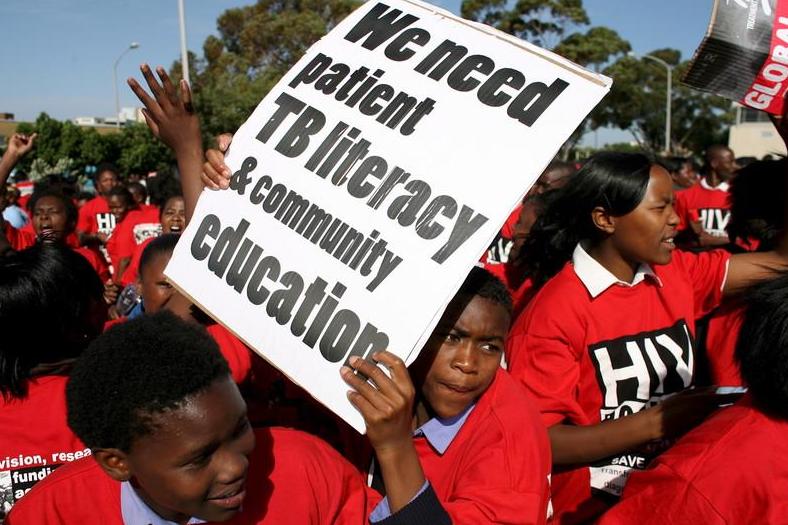
South Africa has shown what political will can accomplish, says Dr Gavin Churchyard, a TB specialist based in Johannesburg. The country once had an abysmal TB preventive therapy programme, with just a few thousand people taking the pills.
But in 2008, after Pakishe Aaron Motsoaledi, then the country’s health minister, made TB prevention a national priority, the numbers began to rise dramatically. By 2011, 350,000 people were enrolled in preventive therapy. Today, South Africa still has the world’s largest TB preventive therapy programme, Churchyard says.
Chaisson did a “back-of-the-envelope” calculation, published in 2017 in The Lancet Global Health, suggesting that if such preventive therapy had been rolled out worldwide, several million deaths could have been averted.
“It makes the deaths that they incurred because of Aids denialism in South Africa look so small,” Churchyard says. “Really, our neglect has cost lives, unfortunately. And it’s time – just as there was a time to end Aids denialism, it’s time to end the TB denialism.”
© The New York Times
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments