When I heard the survival rate for ovarian cancer, I took my treatment into my own hands
When Susan Lisovicz’s stomach pain turned out to be late stage ovarian cancer, the odds were impossible. Opting for the ‘mother of all surgeries’ was just one part of recovery. True survival is about being your own best advocate, she says

I’m glad I was lying down when the doctor told me the true cause of my stomach pains.
“Well, you’ve got a tumour,” were his first words to me. I had just woken up in a hospital bed on the morning after emergency surgery. It was Tuesday 31 October 2017. Halloween.
The doctor’s scary outlook came after two agonising trips to the emergency room that had begun the preceding Friday night. After looking at abdominal X-rays, an ER doctor said constipation was making me feel as though a drawer full of forks was trying to pierce through my belly. He recommended an over-the-counter laxative.
By Saturday evening I was throwing up, and the pain was still relentless. I went back to the ER Sunday, where I was treated with additional laxatives and the first of five enemas. Finally a gastrointestinal specialist, whom my partner had texted in desperation, came on board Monday and performed a partial colonoscopy, then called in the surgeon after discovering that a tumour was causing a nearly complete blockage of my large intestine.
The tumour turned out to be stage three ovarian cancer. It also created another life-threatening situation: the imminent possibility that my colon would rupture. The surgeon relieved the obstruction by performing a temporary colostomy, in which a piece of the colon is diverted to an artificial opening in the abdomen.
The doctor told me he had left the tumour for another day, for which I am forever grateful because this gave me the opportunity to consult with specialists on how to proceed.
I am grateful for the outstanding medical care that helped save my life. But that is not enough. You need to be an active participant – body and mind – in fighting cancer
Ovarian cancer will kill an estimated 14,000 American women this year. Mine was advanced. Stage three means that cancer cells have spread to tissues outside the pelvis or to lymph nodes in the back of the abdomen. Most women diagnosed with stage three ovarian cancer have a five-year survival rate of 39 per cent. With statistics like that, I instinctively knew I would opt for an aggressive response and, ultimately, experimental treatment.
You never know how you are going to react when you hear something so devastating. I had been healthy all my life and was literally standing on my head in a 6 am yoga class the day before everything turned upside down in the ER.
All that slow, deep yoga breathing helped keep me calm – and so did my experience as a journalist. I’d covered my share of complicated stories during my 25 years at CNN and CNBC. The ability to line up experts and to make sense of what they’re saying in a short amount of time is deeply ingrained. And I felt as though I was on deadline now.
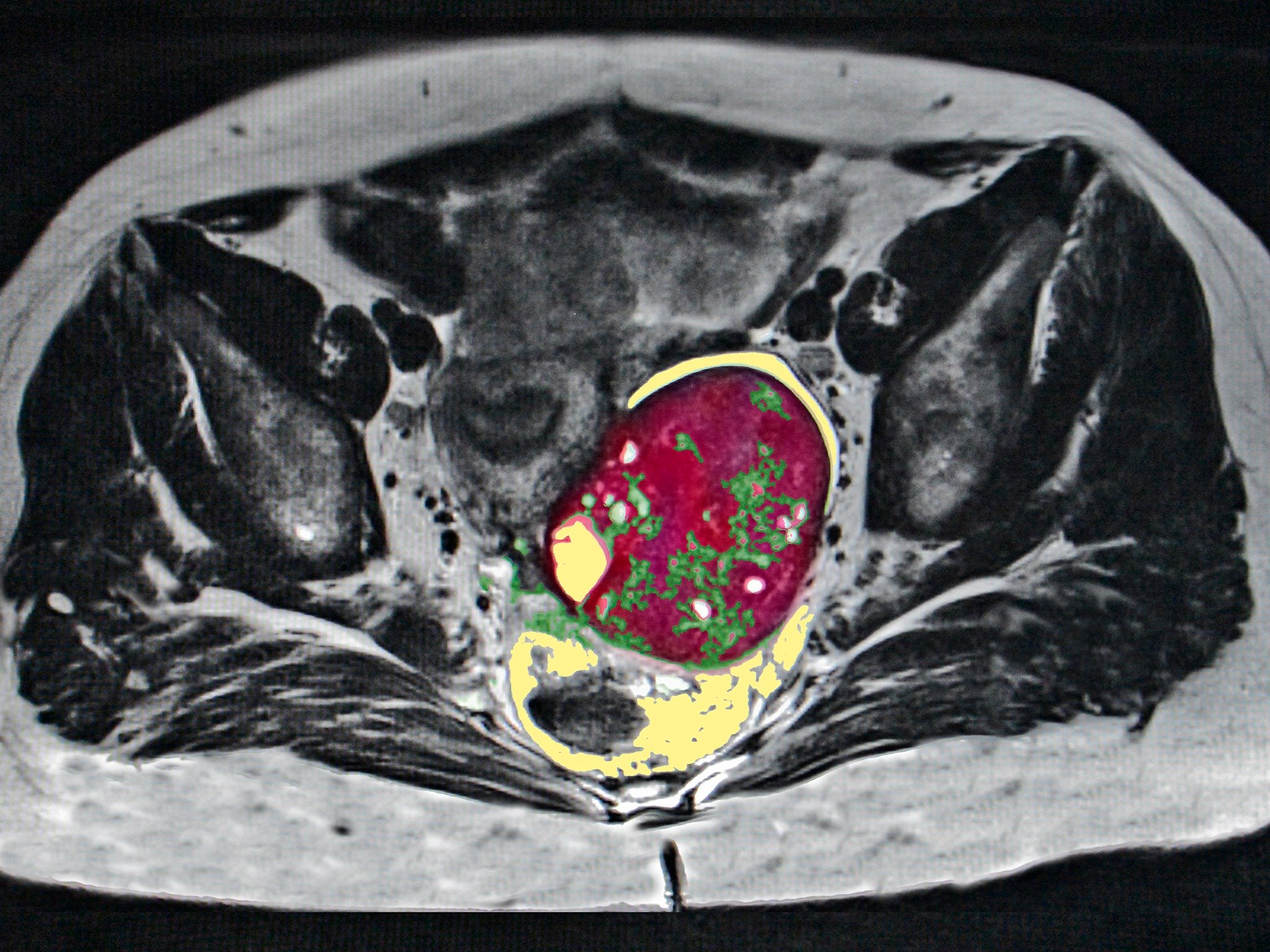
Cancer can move quickly. I wanted my cancer OUT. I wanted it eviscerated. That ultimately meant a drive out of the New York metropolitan area to Baltimore’s Mercy Medical Centre. A family friend had told me about the surgical oncologist Armando Sardi, who has performed nearly 600 cytoreductive surgeries.
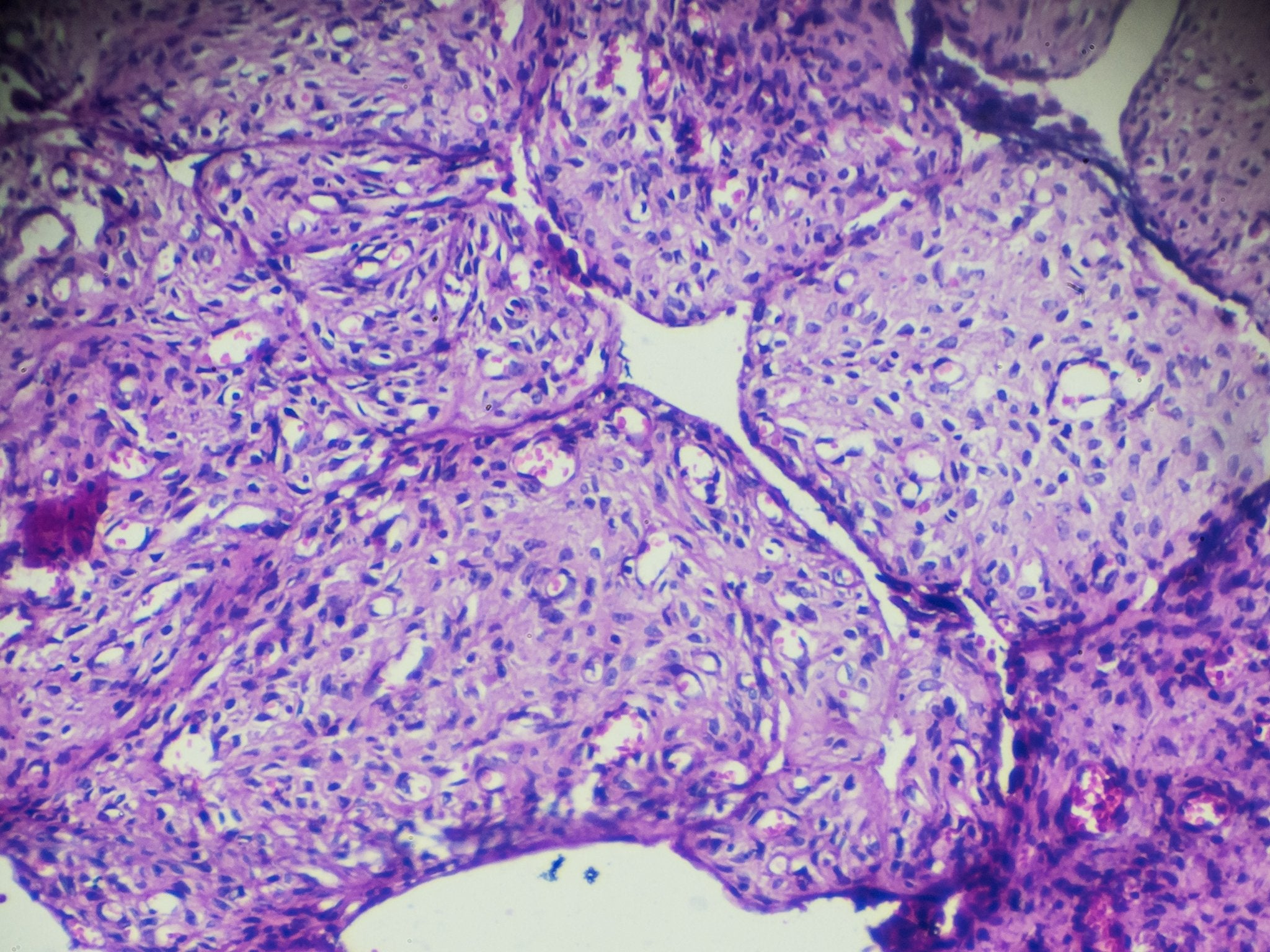
CRS is the aggressive removal or destruction of all or most of the visible tumours in the abdomen. It may also include removal of multiple organs. Some people who have been through it call it MOAS – for “mother of all surgeries.” They are complex, meticulous and long surgeries. Sardi says his longest was 19 hours; his average is seven to 10.
The ability to line up experts and to make sense of what they’re saying in a short amount of time is deeply ingrained. And I felt as though I was on deadline now
I also wanted something else that can come immediately after this surgery: heated chemotherapy on the operating table.
Because it is likely that microscopic disease still remains after surgery, hyperthermic intraperitoneal chemotherapy, or HIPEC, is used to deliver treatment directly to cancer cells in the abdomen. It is believed that heating the solution – in my case, to 107.5 degrees – may improve the absorption of the drugs.
HIPEC has been used for years in some abdominal cancers, but researchers are just beginning to test it on advanced ovarian cancer. Mercy says it is the only US institution investigating CRS with HIPEC in women newly diagnosed with ovarian cancer to see if it could be a new standard of care.
One surgical oncologist, whose hospital did not offer HIPEC in newly diagnosed cases like mine, told me during consultation that heated chemotherapy was the “cherry on the cake”, that impeccable surgery was what really counted. Well, I wanted the cake AND the cherry on the top.
The anaesthesia began at 7.39am on30 November. The surgery ended at 7.37pm. During that time, Sardi and gynaecologic oncologist Teresa Diaz-Montes performed a complete hysterectomy, removed my gallbladder, spleen and the fatty tissue that covers the intestines and organs in the abdomen known as the omentum, cut out about a third of my stomach and about three feet of small bowel and reversed the colostomy. All visible traces of cancer were removed.
“We pretty much peeled off the inside of the belly,” Sardi says. MOAS, indeed. And then I had the 90-minute chemo bath. No, I was not expecting THAT big of a surgery beforehand, but neither was Sardi. “Until I am in surgery, it is unpredictable and the CAT scan usually shows less than what is found,” he says.
It took me more than two months before I had the nerve to read the chilling pathological report and operative note. “You had massive disease,” Sardi told me in a recent phone call. “The good thing is, we were able to take it out.”
I have had no complications. I was released from the hospital nine days after surgery and then stayed in an apartment nearby for another 11 days. Then the staples from my 12 inch scar were removed and I went home to celebrate Christmas with my family. Sardi says there were only about 10 facilities in the world that did CRS/HIPEC when he began doing it in 1994. While many more places offer it now, it is still not mainstream.
A Dutch study published in January in The New England Journal of Medicine shows that patients with advanced ovarian cancer who were treated with HIPEC had longer recurrence-free survival than those who received surgery alone, and they did not experience higher rates of side effects. The stats are still bleak – the median overall survival was 45.7 months in the surgery-plus-HIPEC group vs 33.9 months in the surgery alone group – but that is almost a year’s difference of life. I’ll take that.
The single most motivating thing I read before surgery was a 2013 study that said nearly two-thirds of women with ovarian cancer received substandard care, which is linked to reduced survival rates and underscored the urgency of being your own best advocate. This is just unacceptable for the fifth-leading cause of cancer for women.
Also unacceptable is the fact that there is still no test to catch ovarian cancer early. The vast majority of cases are diagnosed at stage three or four, so getting it right from the outset is critical. You simply have less time for mistakes.
Patients need to “ask the provider and hospital how many ovarian cancer patients they treat, how many ovarian cancer surgeries they perform and their ovarian cancer patients’ rate of survival”, says Robert E Bristow, director of gynaecologic oncology at the University of California Irvine Medical Centre and the lead author of the 2013 study.
A common approach to treating ovarian cancer is chemo to shrink the tumour, followed by surgery. One gynaecologic oncologist advised me to take that route. He outright dismissed HIPEC.
“It’s not the standard of care,” he said. “If it was, we’d all be doing it.” He frowned upon having such a big operation just one month after my emergency surgery. He has a point. Because CRS often involves the removal of multiple organs, there are additional risks, including bleeding, infection and even death. The chemo immediately afterward adds to the danger.
Hey, when you’ve got cancer, you don’t sweat the small stuff. I wore the dress during my vows in municipal court with the tag still attached
“If you don’t know what you’re doing, the mortality can be very high,” Sardi says.
A 2012 study in the Annals of Surgery said that CRS and HIPEC have a “steep learning curve requiring 140 procedures to acquire expertise”.
Diaz-Montes says she and Sardi have worked together so frequently that they often did not need to speak during the long operation. “It’s as if we’re dancing,” she says.
There are also financial factors to consider. While HIPEC is standard of care for appendix cancer, peritoneal carcinomatosis and mesothelioma tumours, it is considered “investigational” for ovarian cancer, says Yolanda Brockington, HIPEC coordinator at the Institute for Cancer Care at Mercy. Many insurance companies don’t pay for that portion of the procedure, which costs $5,000 (£3,800), Brockington says.

Mercy performs two or three CRS/HIPEC surgeries a week, according to Michelle Sittig, an oncology research coordinator at the hospital. That modest number is due in part to the length of the surgeries.
“You have to have the stamina to do it and not give up,” Sardi says.
After seven weeks of recovery from surgery, I began an aggressive round of chemotherapy at New York’s Memorial Sloan Kettering Cancer Centre. Eighteen weeks. Every. Damn. Week. My oncologist there, Carol Aghajanian, said she would manage the worst side effect – nausea – with a pre-chemo IV. Not once was I nauseous. But there is still no cocktail for the humbling fatigue synonymous with chemo. My signature achievement on a few days was simply changing out of my pyjamas before dark.
But then I would look at the lab results, and I wanted to shout from the rooftops. My CA-125, a cancer biomarker, has been 10 or below since January. Normal is 35 and under. It was just over 300 when I was diagnosed in early November.
“It’s as good as it gets,” Aghajanian says.
I am grateful for the outstanding medical care that helped save my life. But that is not enough. You need to be an active participant – body and mind – in fighting cancer. You’re supposed to stay positive. So I got married in the 31-day window between surgeries. My partner proposed at a time when I was forced to carry a bag of my own waste on my stomach and faced a colossal surgery. Now that’s my idea of (Prince) Valiant.
I wore an oatmeal woolen Eileen Fisher dress that I had ordered online a few days before. It was loose enough to cover the temporary colostomy, and it was perfect – except for the plastic magnetic tag that the store had forgotten to remove before shipping. I didn’t see it when I first tried it on. Hey, when you’ve got cancer, you don’t sweat the small stuff. I wore the dress during my vows in municipal court with the tag still attached.

For a couple of hours in the morning there was champagne and laughter. And then by early afternoon I was back in a hoodie and leggings on the subway for a callback on my mammograms, the first time I had ever been called back. I went alone by choice, and as I was riding on the Q train, I thought there is NO WAY I could be told bad news on my wedding day.
I took my place with about a dozen other women, all of us in our blue and white seersucker robes. When the technician called me back for the screening, I told her that I had literally just gotten married. She said, “You mean there’s still hope for me?”
Hope. It’s so important, whatever our priorities might be. She took exactly one picture. That was the closer look that was needed. I was clean.
Ovarian cancer is a disease with a high recurrence rate. “You had the right operation that will give you the best chance,” Sardi tells me.
On my last day of treatment on 15 May, my chemo nurse, a breast cancer survivor, said, “I never ever want to see you here again.”
My CT scan on 11 June was “beautiful, crystal clear”, according to Aghajanian.
Now I hope to return fully to an active and purposeful life, which often begins with sunrise headstands – and may include a honeymoon.
© The Washington Post
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks