Open wounds converted into healthy skin in scientific first
'This observation suggests that we could potentially cover or heal a wound of any size in a specific time frame,' Prof Juan Carlos Izpisua Belmonte tells The Independent
Scientists have shown it is possible to directly regrow healthy skin in life-threatening open wounds caused by burns or ulcers that would previously only be treatable with surgical grafts.
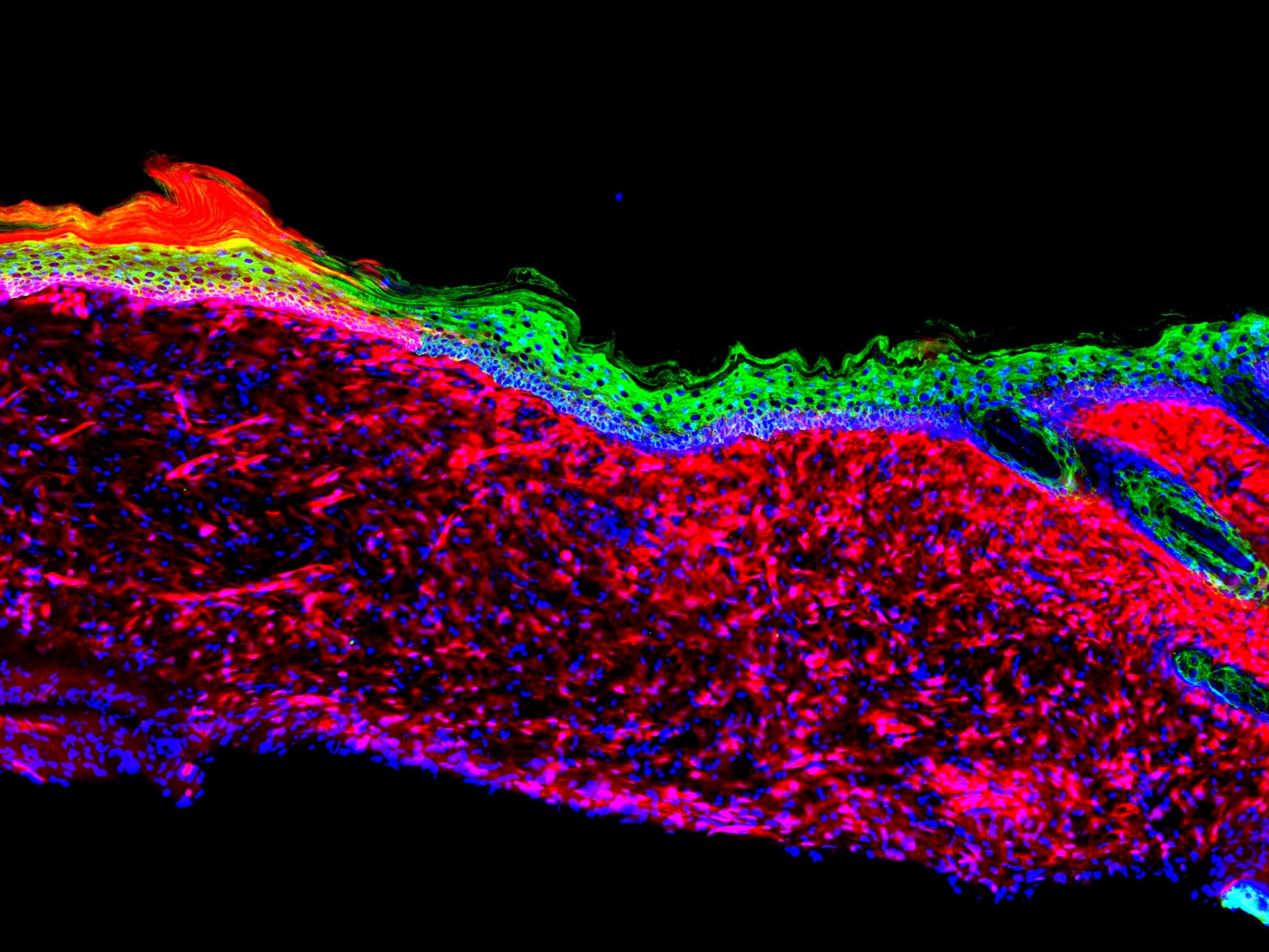
Four key cellular ingredients which skin cells need to begin regenerating the complex layers that form the body’s outer protective barrier have been identified by academics at the Salk Institute in San Diego.
While large wounds have lost the base layer of skin cells they need to regenerate, the team used viruses to reprogramme other cells in the wound and connective tissue below to create these four proteins.
They managed to form new skin within 18 days.
The findings could lead to a new generation of simple wound treatments which could prevent complications from hard-to-heal wounds that are common among older people and patients with diabetes.
It may also allow for the repair of other organ damage, although this would likely be some time in the future.
However, although the study demonstrated it’s possible in mice, further refinements are needed before it reaches hospitals.
“What we did in the current study is generate three-dimensional skin coverage in an experimental open wound setting in which no coverage or healing would ever be possible,” Professor Juan Carlos Izpisua Belmonte, one of the study’s senior authors, told The Independent.
“This observation suggests that we could potentially cover or heal a wound of any size in a specific time frame.”
He added: “Though this is not specifically examined in our current work, some of our findings suggest that our reprogramming technology has the potential to return aged or somewhat unhealthy skin back to a more ‘youthful’ state.”
To heal a wound, cells called keratinocytes, which make the outer layers of the skin, need to move in and gradually seal the damaged areas. However this healing process is diminished by age, and in people with circulatory conditions that can be caused by things like smoking or diabetes.
In these cases small wounds can become large unhealing “ulcers” which can have deadly complications. Pressure ulcers in the UK alone affect 700,000 people a year and cost the NHS £3.8m a day.
Ulcers, burns and other wounds which damage multiple layers of skin or are too large may need treatment with a skin graft, usually by taking skin from another part of the body to transplant.
Where there is not enough healthy skin to take, doctors may use some skin stem cells to grow them in the lab and create a prosthetic transplant – however this is very costly and slow and patients are vulnerable in the meantime.
But Professor Izpisua Belmonte and his team set out to find a better alternative.
“We set out to make skin where there was no skin to start with,” said Masakazu Kurita, a research associate at Salk and lead author of the study published in the journal Nature.
They focused on keratinocytes’ ability to act like skin stem cells – the cell types which can change into any type of tissue.
While large wounds where the base layer of skin has been lost have no keratinocytes to regrow the tissue, the researchers thought it might be possible to reprogramme other cells from the connective tissue beneath.
Looking at the cellular products of keratinocyte and wound cells, they identified 55 protein molecules which are important in the skin regrowth, before whittling it down to four key proteins with trial and error.
They then found the genetic instructions the cells use to make these proteins and loaded them into retroviruses, which can write their genetic material into cells, before applying them to non-healing ulcers on mice.
After two and a half weeks the wounds had a complex layer of skin that knitted itself into the edges of the healthy tissue, and within six months these new cells were identical on a cellular level to the original skin.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks