Regeneron: What is the new coronavirus antibody treatment and how will it help Covid patients?
UK trial shows antibody cocktail reduces deaths in people who have not mounted own immune response
Researchers have found a new treatment with the first antiviral drug shown to save lives in severely-ill coronavirus patients admitted to hospital.
The Recovery trial demonstrated the antibody combination developed by Regeneron reduced the risk of death when given to patients with severe Covid-19 who had not mounted a natural antibody response of their own.
The results could pave the way for Regeneron’s monoclonal antibody treatment to be approved by UK regulators and rolled out for use across the NHS.
Here are your questions answered from the latest update from the Recovery trial:
What has the trial found?
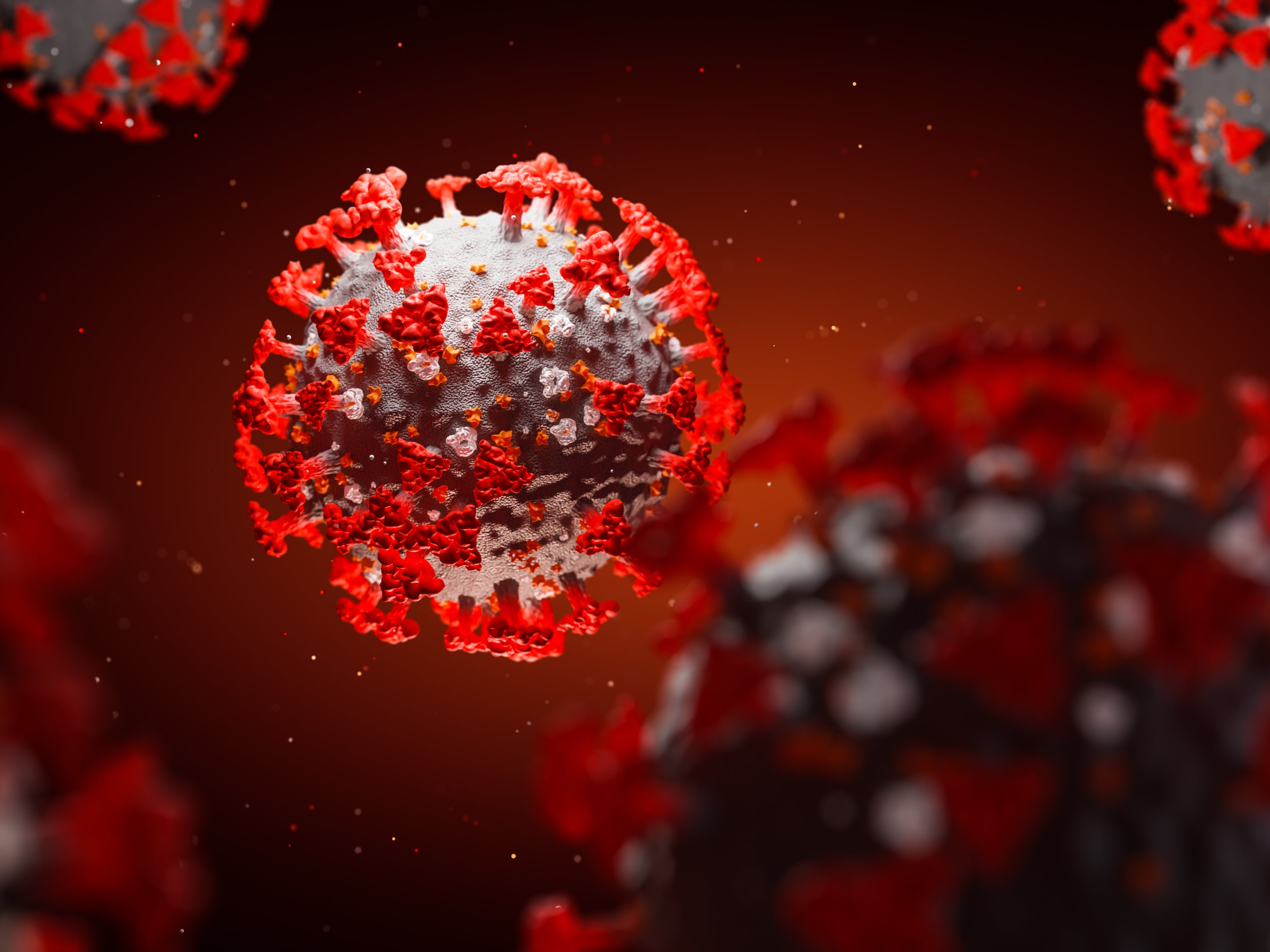
Researchers were examining a type of treatment called a monoclonal antibody combination – which has been previously called an “antibody cocktail”.
They found taking the treatment, made by pharmaceutical company Regeneron, reduces deaths for patients in hospital with Covid-19 who have not mounted their own immune response.
What is this treatment and how does it work?
The therapy uses two artificial antibodies; these are generated in a lab to make very potent antibodies.
These two monoclonal antibodies, casirivimab and imdevimab, bind specifically to two different sites on the coronavirus spike protein, neutralising the ability of the virus to infect cells.
The idea is to inject these artificial antibodies so they bind to the virus in a bid to stop the infection in its tracks.
Because this treatment uses two types of artificial antibodies, it is hoped it will be able to bypass any resistance the patient builds up against one of them.
It is also hoped by using a combination of antibodies, the likelihood of viral variants to escape treatment is diminished.

Would this be given to all patients?
No, this study implies patients who do not have antibodies would benefit from this treatment, not patients who already have antibodies.
As the researchers say: “If they have (got antibodies), there’s no need to give them more.”
If patients do not have antibodies of their own, then giving them this combination of two artificial antibodies, via an intravenous infusion (also known as an IV drip), reduces their chances of dying.
What is the benefit?
This is an important study because it assessed the treatment among some of the sickest Covid patients and gave them better odds of survival.
They were also found to spend fewer days in hospital compared to those who didn’t get the treatment. It was also found to reduce their chances of needing to be treated with a ventilator.
What about other treatments?
Dexamethasone and Tocilizumab are used for treating Covid-19, but these are both therapies that tackle the immune response – the body’s overdrive inflammatory reaction to the virus.
Researchers say this is the first time we have a treatment that is actually targeting the virus itself.
The new therapy could be used in combination with other treatments.
Who does not have antibodies?
Some cancer patients, people with compromised immune systems and some others who fail to make an antibody response.
Having antibodies in the blood shows that a person’s body has created an immune response – either as a response to infection or a vaccine.
But the Covid-19 vaccines are not completely effective so some people may have both doses and still get sick.
Will people start to receive it straight away?
No, before it becomes part of standard practice it will need to go through regulatory approval from the Medicines and Healthcare products Regulatory Agency (MHRA).
Meanwhile, it will take some forethought from the NHS before it is rolled out as it will require patients to be tested to see if they have antibodies when they are admitted to hospital – which is not currently standard practise.
While antibodies are usually assessed in labs, it is hoped that quicker lateral-flow tests could be used for screening antibody status when patients are admitted to hospital for a quick result.
What is the cost?
Researchers said they are not aware of exact costs but the treatments needed “intensive” manufacture, it could cost around £1,000 or £2,000 for the one-off treatment.
Additional reporting by PA
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments



Bookmark popover
Removed from bookmarks