LSD and magic mushrooms could heal damaged brain cells in people suffering from depression, study shows
Psychedelics could be 'next generation' of safer treatments for mental health
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Psychedelic drugs like LSD and ecstasy ingredient MDMA have been shown to stimulate the growth of new branches and connections between brain cells which could help address conditions like depression and addiction.
Researchers in California have demonstrated these substances, banned as illicit drugs in many countries, are capable of rewiring parts of the brain in a way that lasts well beyond the drugs' effects.
This means psychedelics could be the "next generation" of treatments for mental health disorders which could be more effective and safer than existing options, the study's authors from the University of California.
In previous studies by the same team, a single dose of DMT, the key ingredient in ayahuasca medicinal brews of Amazonian tribes, has been shown to help rats overcome a fear of electric shock meant to emulate post-traumatic stress disorder (PTSD).
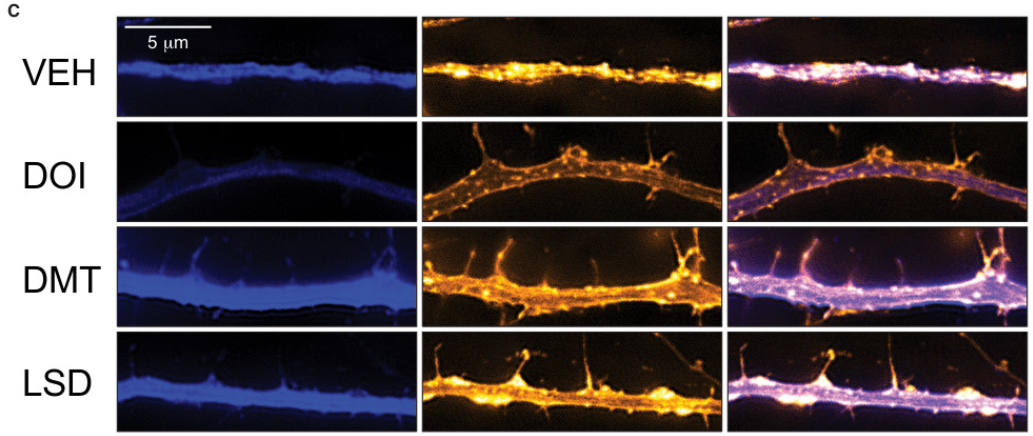
Now they have shown this dose increases the number of branch-like dendrites sprouting from nerve cells in the rat's brain.
These dendrites end at synapses where their electrical impulses are passed on to other nerve cells and underpin all brain activity. But they can atrophy and draw back in people with mental health conditions.
“One of the hallmarks of depression is that the neurites in the prefrontal cortex – a key brain region that regulates emotion, mood, and anxiety – those neurites tend to shrivel up,” says Dr David Olson, who lead the research team.
These brain changes also appear in cases of anxiety, addiction, and post-traumatic stress disorder and stimulating them to reconnect could help to address this.
The research, published in the journal Cell Reports today, looked at drugs in several classes including tryptamines, DMT and magic mushrooms; amphetamines, including MDMA; and ergolines, like LSD.
In tests on human brain cells in the lab, flies and rats, it found these substances consistently boosted brain connections.
Dr Olson compared the effects to ketamine, another illicit drug which represents one of the most important new treatments for depression in a generation, and found many psychedelics have equal or greater effects.
A ketamine nasal spray is being fast-tracked through clinical trials after it was shown to rapidly relieve major depression and suicidal thoughts in people who cannot be helped by other treatments.
However its use has to be weighed against its potential for abuse, and its ability to cause a form of drug-induced psychosis.
“The rapid effects of ketamine on mood and plasticity are truly astounding,” said Dr Olson. “The big question we were trying to answer was whether or not other compounds are capable of doing what ketamine does.”
“People have long assumed that psychedelics are capable of altering neuronal structure, but this is the first study that clearly and unambiguously supports that hypothesis."
The fact that many of these drugs seem to mimic the groundbreaking benefits of ketamine opens up an array of new treatment options, which may be less open to abuse, if these drugs can make it to clinical trials.
Dr Olson said: “Ketamine is no longer our only option. Our work demonstrates that there are a number of distinct chemical scaffolds capable of promoting plasticity like ketamine, providing additional opportunities for medicinal chemists to develop safer and more effective alternatives.”
The news that yet more banned substances could help tackle serious and debilitating disease comes as the UK Home Office is embroiled in a row over medicinal cannabis in treating epilepsy.
After months seizure-free, 12-year-old Billy Caldwell had a seizure last night after airport customs officials confiscated his prescription from Canada.
Billy had previously had the UK’s only NHS medical cannabis prescription, for an oil which banished seizures that used to strike 100 times a day, but the Home Office intervened to block his GP from prescribing it.

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments