Lab-grown blood used for human transfusion in world first
World’s first clinical test hailed as ‘huge stepping stone’
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
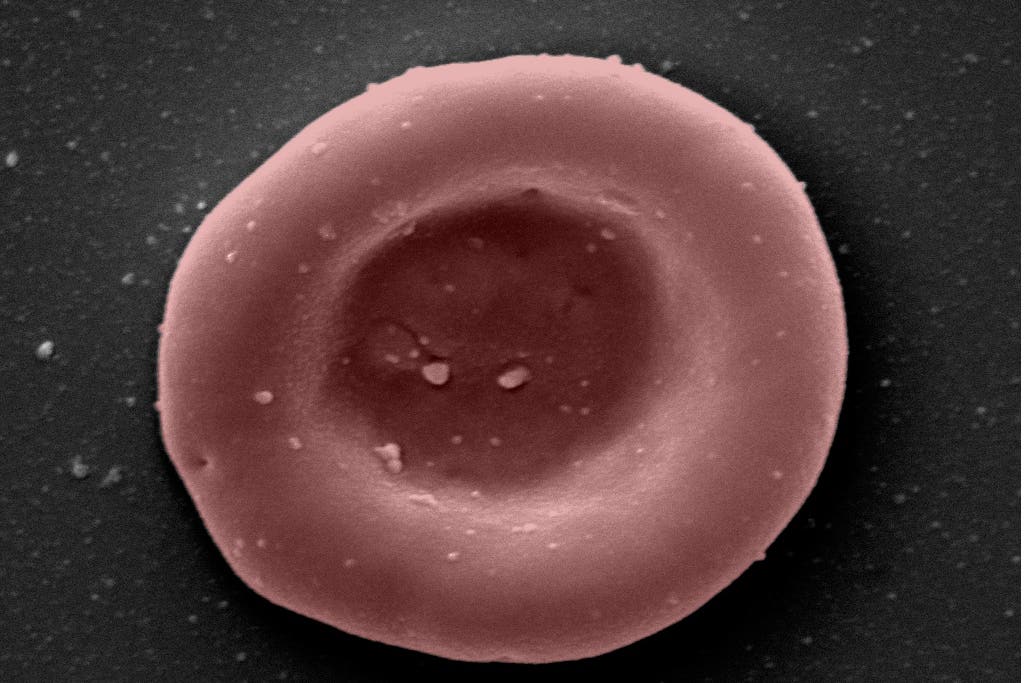
Your support makes all the difference.Blood grown in a laboratory has been transfused into two volunteers in the world’s first clinical trials that will likely revolutionise treatments for patients with rare blood types or sickle cell disease.
The lab-manufactured blood cells were grown from stem cells from donors and were transfused in quantities of around 5-10ml – about one to two teaspoons – into volunteers.
The trial is to study the lifespan of the lab-grown cells versus infusions of standard red blood cells from the same donor.
It is expected that the lab-grown blood cells will perform better than standard donated red cells as the manufactured blood cells are fresh, meaning patients who regularly need blood may not need transfusions as often.
“This challenging and exciting trial is a huge stepping stone for manufacturing blood from stem cells,” said Ashley Toye, professor of cell biology at the University of Bristol and director of the NIHR Blood and Transplant Unit in red cell products.
“This is the first-time lab grown blood from an allogeneic donor has been transfused and we are excited to see how well the cells perform at the end of the clinical trial.”
The patients were closely monitored and no untoward side effects were reported. They are healthy and doing well, researchers said.
If the manufactured cells last longer in the body and patients require less transfusion, it would reduce the iron overload from frequent blood transfusions, something that can lead to serious complications.
“We hope our lab grown red blood cells will last longer than those that come from blood donors,” said Cedric Ghevaert, professor in transfusion medicine and consultant haematologist at the University of Cambridge and NHS Blood and Transplant (NHSBT).
“If our trial, the first such in the world, is successful, it will mean that patients who currently require regular long-term blood transfusions will need fewer transfusions in future, helping transform their care.”
Donors from NHSBT’s blood donor base donated blood for the trial and stem cells were separated from their blood.
These stem cells were then grown to produce red blood cells in a laboratory at NHSBT’s Advanced Therapies Unit in Bristol.
Those who received the blood are healthy members of the National Institute for Health and Care Research (NIHR) BioResource.
At least 10 volunteers are expected to receive two mini transfusions at least four months apart, which will include one of standard donated red cells and one of lab grown red cells.
This will allow scientists to study if young red blood cells made in the laboratory last longer than cells made in the body.
“Patients who need regular or intermittent blood transfusions may develop antibodies against minor blood groups which makes it harder to find donor blood which can be transfused without the risk of a potentially life-threatening reaction,” said Dr Farrukh Shah, NHSBT’s medical director of transfusion.
“This world leading research lays the groundwork for the manufacture of red blood cells that can safely be used to transfuse people with disorders like sickle cell.
“The need for normal blood donations to provide the vast majority of blood will remain. But the potential for this work to benefit hard to transfuse patients is very significant.”
More trials are required before its clinical use in patients. However, scientists explained that this research was a significant step towards the future of using manufactured red blood cells to improve treatments in patients with rare blood types or people with complex transfusion needs.





Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments