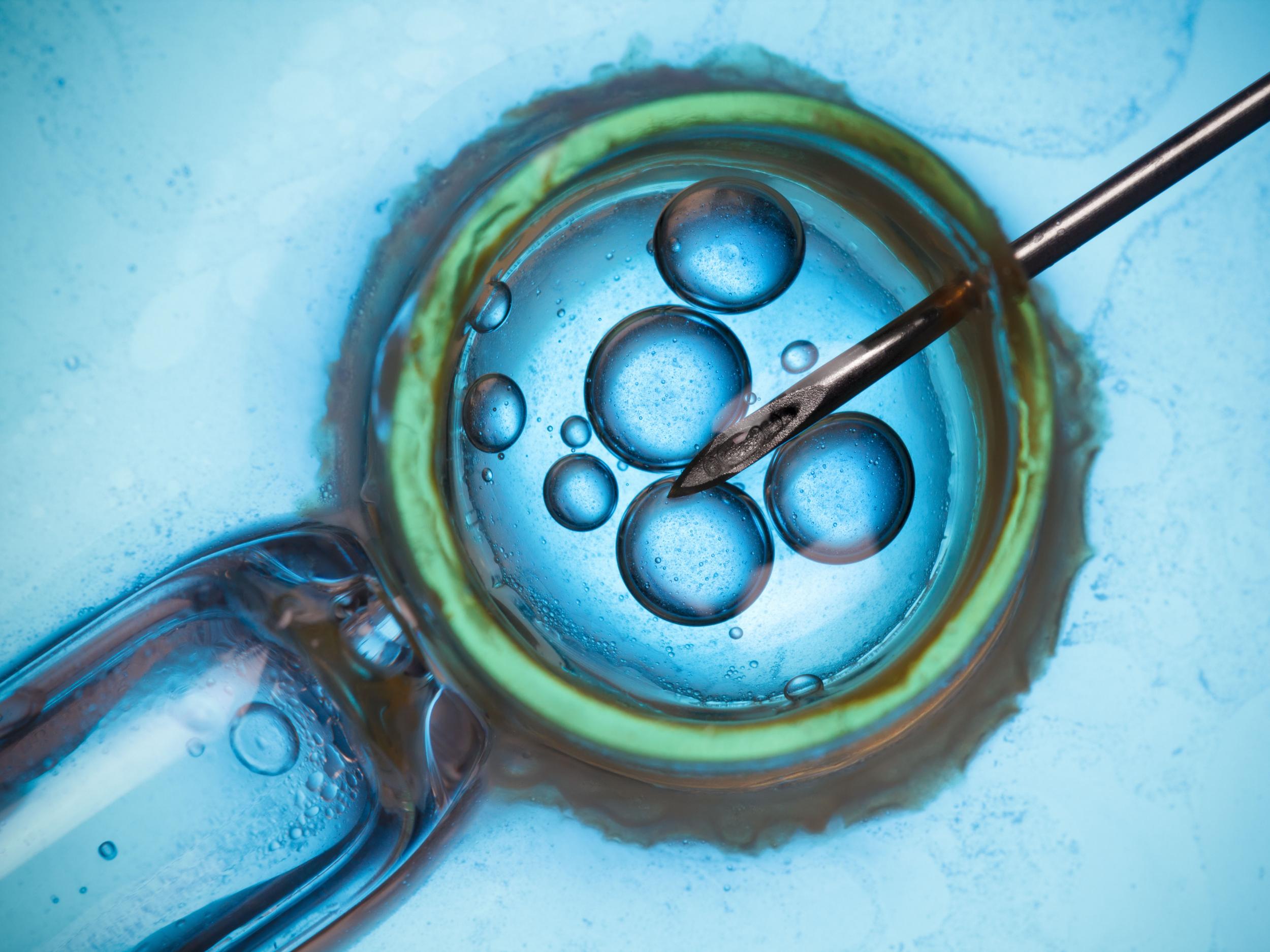
Couples being denied IVF treatment on NHS because men are deemed overweight or too old, campaigners say
More than a quarter of CCGs use man’s BMI to determine whether they can be referred for fertility treatment, according to audit by Fertility Fairness
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A man’s weight, age and other “arbitrary criteria” should not be used to ration access to NHS fertility services such as IVF, a campaign group has said.
Fertility Fairness said England’s Clinical Commission Groups (CCGs) are rationing access to NHS fertility services by setting their own access criteria, including male body mass index (BMI) and age.
It said these criteria do not form part of the National Institute of Health and Clinical Excellence’s (Nice) fertility guidelines and should not be used to determine who can or cannot be referred for IVF or intracytoplasmic sperm injection (ICSI).
Fertility Fairness said its 2018 audit of England’s 195 CCGs reveals that more than a quarter (27 per cent) now use a man’s BMI to determine whether a couple can be referred for IVF on the NHS.
Fourteen CCGs (8 per cent) stipulate men must be aged below 55 in order to have NHS fertility treatment.
A quarter of CCGs insist a woman’s anti-Mullerian hormone (AMH) level and/or antral follicle count (AFC) is at a specific level, and 91 per cent do not allow couples to access IVF on the NHS if one of the couple has a child from a previous relationship, which it described as social rationing.
As well as introducing extra “access to NHS IVF” criteria, the vast majority of CCGs (87 per cent) ration NHS fertility services by refusing to provide the recommended three full IVF cycles, the group added.
Nice recommends government funding for three full IVF cycles, but funding varies across the country and access is often described as a postcode lottery.
It means six out of 10 IVF cycles in the UK are funded by patients themselves, according to the the Royal College of Obstetricians and Gynaecologists (RCOG).
Fertility Fairness said seven CCGs (3.6 per cent) have removed NHS IVF entirely (all are in the south), while 20 per cent offer one full IVF cycle and 40 per cent offer only one partial IVF cycle (transferring a finite number of embryos).
Fewer than a quarter (23 per cent) offer two IVF cycles, it said.
In the last two years, 30 CCGs (15.3 per cent) have slashed NHS fertility services, and one in 10 is currently consulting on cutting or removing NHS fertility treatment.
Fertility Fairness co-chairwoman Sarah Norcross said: “It is shocking to see CCGs introducing their own ‘access to IVF’ criteria, as well as reducing the number of IVF cycles they offer.
“It is not the CCG’s job to decide the criteria for accessing NHS fertility services.
“Nice has accessed the evidence in its guidelines and developed access criteria for NHS patients and they do not include male BMI, male age, a woman’s AMH level or whether or not a couple has a child from a previous relationship.
“What criteria will CCGs introduce next – star signs and shoe size? CCGs need to remove their extra ‘access to IVF’ criteria now.”
Nice recommends that IVF should be offered to women under the age of 43 who have been trying to get pregnant through regular unprotected sex for two years, or who have had 12 cycles of artificial insemination.
But the final decision about who can have NHS-funded IVF in England is made by CCGs, and their criteria may be stricter than those recommended by Nice.
Aileen Feeney, co-chairwoman of Fertility Fairness and chief executive of the charity Fertility Network UK, said: “Fertility Network is extremely concerned about the effect that reducing access to NHS IVF has on already distressed patients.
“Infertility is a devastating disease causing depression, suicidal feelings, relationship breakdown and social isolation; removing the recommended clinical help or making it harder to access is cruel and economically short-sighted.
“Access to NHS treatment should be according to medical need and not your postcode.”
She added that anyone affected can join Fertility Network’s #Scream4IVF campaign, which is calling for fair access to IVF in the UK.
An NHS England spokesman said: “Ultimately these are decisions for local GPs who rightly decide how best to balance the various competing demands on the NHS.”
This comes as the Victoria Derbyshire programme found women over 34 are automatically being refused IVF treatment on the NHS in 12 areas of England.
While guidelines say IVF should be offered to women until age 42, new figures show around 80 per cent of areas are failing to do this.
Ms Norcross told the programme it “penalises the women who take longer to find a partner or wish to put themselves on a secure financial footing before trying to conceive”.
Press Association
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
3Comments