Electroconvulsive therapy does work – and it can be miraculous
After bouts of tormenting delusion, just one session of ECT can help dilute the hysteria of psychological patients

The use of electroconvulsive therapy (ECT) to treat psychiatric disorders is on the rise in England, according to a new report in The Guardian. There was an 11 per cent rise in the number of procedures performed on the NHS between 2012-13 and 2015-16.
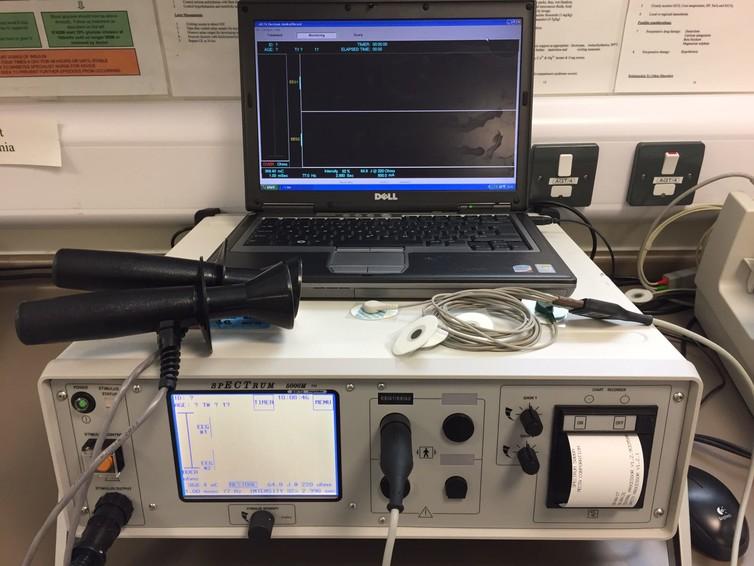
ECT involves passing an electric current through the head of an anaesthetised patient. The aim is to produce an epileptic fit. It is used mostly to treat severe or treatment-resistant depression, but it can also have beneficial effects in some cases of mania and schizophrenia.
Its therapeutic effect was discovered in 1938. Today, it remains the most effective treatment for severe depression. Yet, for some reason, it is always presented in a negative light. Not least in The Guardian’s latest report where it is described as “a crude, controversial treatment, which fell sharply out of favour around the turn of the millennium”. Cue the inevitable debate about the treatment.
Although presented as “exclusive data” in The Guardian, the authors largely reiterate the data collected by the body that monitors ECT in the UK: the ECT Accreditation Service (ECTAS). The data is freely available on the Royal College of Psychiatrists website and counted 2,148 courses of ECT given during 2014-2015.
A quick glance through the ECTAS document can tell us a lot about the nature of the illnesses treated with ECT and the remarkable outcomes: 51.7 per cent of people were rated as “severely ill” and another 18.7 per cent as “among the most severely ill” prior to ECT. At the end of their treatment, however, 74.4 per cent were “much improved/very much improved”, while only 1.7 per cent had deteriorated. This is a treatment reserved for the most severely depressed patients, and it produces unrivalled improvements. Despite this, it is still a treatment that has its passionate opponents.
What does the evidence show?
Let us consider some of the arguments of the opponents. Speaking to The Guardian, Richard Bentall, a professor of clinical psychology at the University of Liverpool, said he “doesn’t believe that there are adequate clinical trials of ECT to establish its effectiveness” and that the design of trials had not been “up to scratch”. In other words, we are not sure that ECT works.
But there have been plenty of trials. A review in The Lancet listed the various ways ECT has been tested over the years. ECT has been compared with stimulated ECT (six trials, all favouring real ECT). ECT has been compared with drugs in 13 trials (11 favoured ECT). Bilateral ECT was more effective than unilateral (that is, treatments given to the whole brain are more effective than those given to half of the brain). And, finally, six trials that compared higher electric charges with lower electric charges found that higher charges produced greater improvements.
Still, every few years the opponents of ECT demand more evidence. In response to such demands, a large study was conducted in the US (the CORE report on 253 patients) and the results were published in 2004. The study set the bar for improvement very high: it required depressed patients to have almost no symptoms on two consecutive measurements at the end of the treatment period. Three-quarters of patients reached those remission criteria. No other treatment in psychiatry has come even close to such effects.
The unrecorded benefits
The real effect of ECT is even stronger than what has been claimed in trials. This is because it produces its best effect in the most severely ill patients: those who stop talking, stop eating or become psychotic.

In psychotic depression – which is characterised by the presence of delusions – the remission rates are the highest, easily topping 80 per cent (the CORE study found 95 per cent remission in psychotic depression). In fact, if a patient with psychotic depression is not improving during an ECT course, as the ECT lead consultant in my hospital, I try to find out what we are doing wrong.
These patients do not get included in randomised trials, as they are not capable of providing informed consent and most professionals would think it unethical to allow them to receive a placebo or any weaker treatment that is compared to ECT. They would be even less likely to receive psychotherapy, as they would be deemed – correctly – as being incapable of engaging in psychological treatments.
I suspect that the opponents of ECT will still reject the evidence from new trials – after all, one can find something “not up to scratch” with anything, if one has already formed a strong belief. Perhaps such people might be persuaded if they go to an ECT clinic and witness one of the miraculous changes that occur there. I do this with medical students who come to observe one session of ECT, as part of their education.
Every few weeks, we have a patient who enters the treatment room mumbling incoherently, or telling us that they are a sinner deserving to be punished, or complaining that they have no intestines or some other vital body part or function. And, after a single bout of ECT, while still in the recovery room, some of these patients start talking coherently and change the topic away from their tormenting delusions. The students come back, after exchanging a few words with the patients, with their jaws dropped and a sense of disbelief in their eyes. This does not happen every day, and usually takes more than one session, but you only need to see it once to remember forever that ECT does work.
The other argument proposed by the opponents is the perceived lack of knowledge about the way ECT works. While it is true that even I tell patients that we are not sure how it works, there are things we can be sure about. For example, we know that ECT works by eliciting an epileptic fit, and that it works better if the fit is stronger. But what happens in the brain as a consequence? Again we do know quite a lot: there is an increase in a number of different neurotransmitters, changes in receptor sensitivity, activation in certain neuronal circuits, and a decrease in connectivity between areas involved in mood regulation.
There are many theories about how ECT works and many of them are quite plausible. And perhaps the reason ECT works so well and so fast is exactly because it produces multiple different therapeutic effects. So our “failure” to point at a single mechanism of action could be due to what might be the strength of this treatment.
And does anybody really think that if we can’t explain why something works, we should not use it? That would mean not using many of the pharmaceuticals on the market today. Drugs regulators, such as the US Food and Drug Administration, only require that a pharmaceuticals firm proves the efficacy of a drug, not provide definitive evidence for how it works.
linical professor at Cardiff University. This article first appeared on The Conversation (theconversation.com)
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks