‘Paradigm shift’ in type 1 diabetes shows new drugs which could delay disease’s emergence
‘Senescent beta cells are like the bad apples that spoil the whole basket,’ expert says. ‘Eliminating the bad apples can save the rest’

Scientists may have been looking in the wrong place for a cure to type 1 diabetes after a new study claims to have found “a paradigm shift” in treatment.
Researchers have found the disease could be kept at bay in animals by clearing out defective insulin-producing cells.
Drug development has previously been focused on preserving these “beta cells” by preventing the immune system wiping them out, but US researchers say their findings turn this on its head.
“This is a paradigm shift for T1 diabetes therapy,” said Professor Anil Bhushan of the University of California, San Francisco, who led the study published in Cell Metabolism. “These data suggest the problem may not be an immune system gone awry. Instead, perhaps therapies should find a way to do the job the immune system is failing to do: clear the senescent cells early on.”
The team found evidence that type 1 diabetics have a problem with the DNA repair that causes beta cells in the pancreas to stop functioning properly and leak signs of damage onto their neighbours – known as secretory senescence.
Prof Bhushan’s team found signs of this DNA damage and secretory senescence in mice, but also in pancreatic tissue donated by six deceased patients with early stage type 1 diabetes, and in living donors with early signs of diabetes.
This suggests they may have identified an early marker of diabetes, but also points to a way to stop it.
Senescent cells, those too old or damaged to function, are usually mopped up by the immune system over time. But in type 1 diabetes researchers found the signs of damage become so widespread the immune system goes into overdrive, destroying the whole insulin-producing structure beyond recovery.
Testing this theory in mice genetically engineered to develop the disease, Prof Bhushan’s team found that the subjects responded to recently approved cancer drug Venetoclax.
This is part of a new class of drugs made to mop up senescent cells which accrue with age and could impact a host of other conditions; in this case they hoped it would prevent the destructive immune response.
In trials, 75 per cent of the animals in the control group developed diabetes by 28 weeks old, but only 30 per cent given a two-week dose of Venetoclax developed the disease, and the healthy beta cells were left untouched by the immune system.
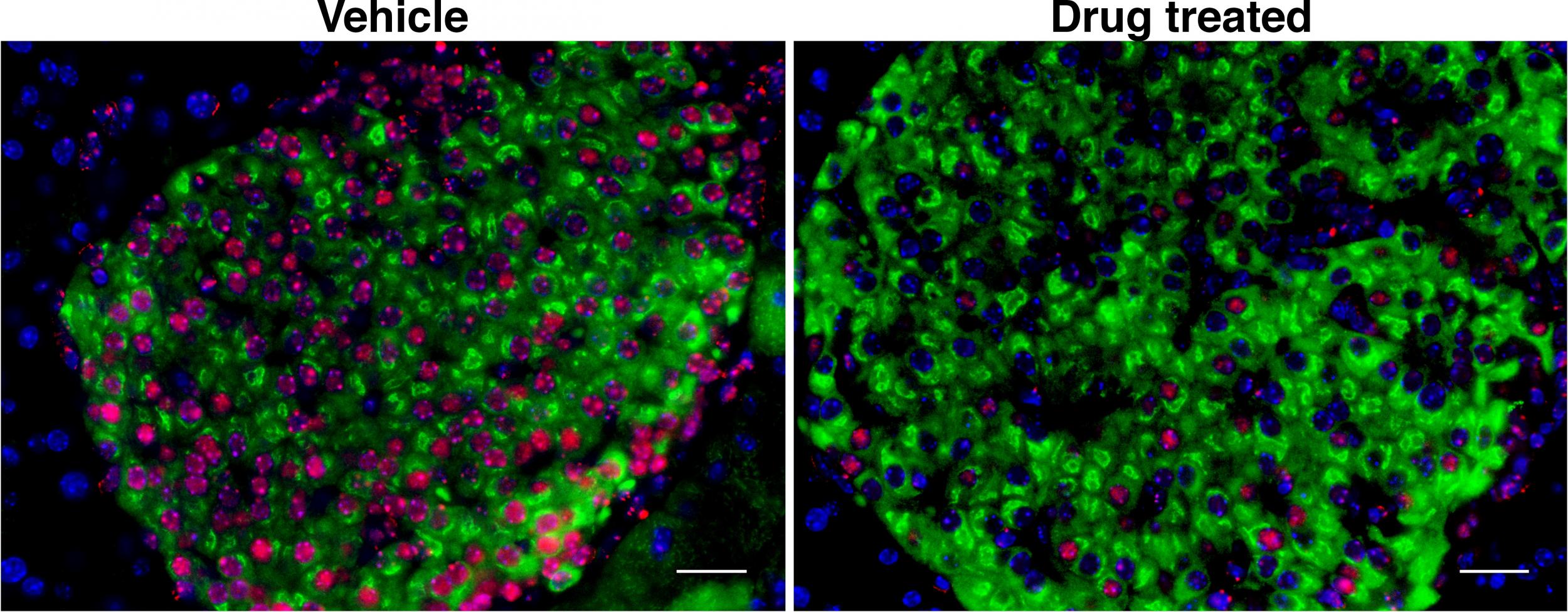
“Here we show that eliminating the bad apples can save the rest, which brings a new therapeutic avenue for treating patients with T1 diabetes,” Dr Ajit Shah, another of the authors, said.
Type 1 diabetes usually emerges by adolescence, and the researchers suggest a future treatment to clear out defective beta cells could push back this date by years.
Around 400,000 people in the UK live with type 1 diabetes, and it can be well managed with insulin injections and blood sugar monitoring.
However, over time it can lead to complications like sight loss and amputations, and average life expectancy is around a decade shorter. While this is improving, new methods to manage or cure the condition could maximise people’s healthy years.
Independent researchers cautioned this was just one result, and the findings with Venetoclax had not been proven in humans, but agreed it was a new and exciting prospect to study.
Professor Naveed Sattar, an expert in metabolic medicine from Glasgow University, said the findings in donated pancreatic cells suggested the results could cross over to humans but it was “early days” and new treatments could take decades.
“Other groups should now urgently aim to replicate these findings, and if they can then future trials of drugs which interfere with this harmful process would seem possible,” he told The Independent.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks