Low-cost drug found to limit lung damage in Covid patients
Drug could have ‘major impact’ in fighting coronavirus, researchers say
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A low-cost drug is safe and effective in limiting lung damage in Covid patients, a new study has found.
Research has shown that Heparin - a widely available and affordable drug - could be used safely to treat Covid, boosting treatment options for patients suffering from severe infections.
Researchers from the Australian National University and King’s College London discovered breathing and oxygen levels improved in 70 per cent of patients after inhaling a course of Heparin.
Heparin is unique as it has anti-viral, anti-inflammatory and anti-coagulant effects which are considered relevant for the treatment of Covid.
Professor Frank van Haren, study lead in the findings, said Heparin could have a “major impact” in the fight against Covid.
“Most Covid experts agree that vaccination alone is not going to stop the pandemic. This could really assist in poorer countries where vaccination is challenging and we think it could help front line workers who could use it as a preventative measure,” Professor van Haren said.
He added: “Inhaled Heparin is a promising new possibility to provide a low-cost, safe and effective treatment for Covid that is available and affordable to low and middle-income countries around the globe.”
The researchers are coordinating further studies tracking hospital patients infected with Sars-CoV-2 in 13 countries who were given doses of inhaled Heparin.
Co-author Professor Clive Page who is co-leading study, from King’s College London, said: “Inhaled Heparin has antiviral properties which work by binding to the spike proteins the coronavirus uses to enter the cells of the body. Inhaled Heparin effectively stops the virus infecting cells in the lungs and could also stop people from getting the virus from others.
“It also works as an anti-inflammatory drug - the medicine has the ability to calm everything down when the body is mounting an exaggerated response to the virus. We already know heparin can reduce lung damage caused by this inflammation and the immune response overdrive that we see in other lung diseases which could provide benefit to patients hospitalised with Covid.”
He added: “There is no other drug that has these three different effects - anti-viral, anti-inflammatory and anti-coagulant.”
Patients with severe Covid develop blood clots in the lungs which can be lethal. Blood thinners, such as Heparin, can prevent such clots from forming.
Because the drug has antiviral properties and calms the immune system, it can be used at different stages of treatment. Indeed, treated patients included in the studies were not uniform in their Covid disease severity, which suggests inhaled Heparin is safe and effective to use across the spectrum of Covid disease.
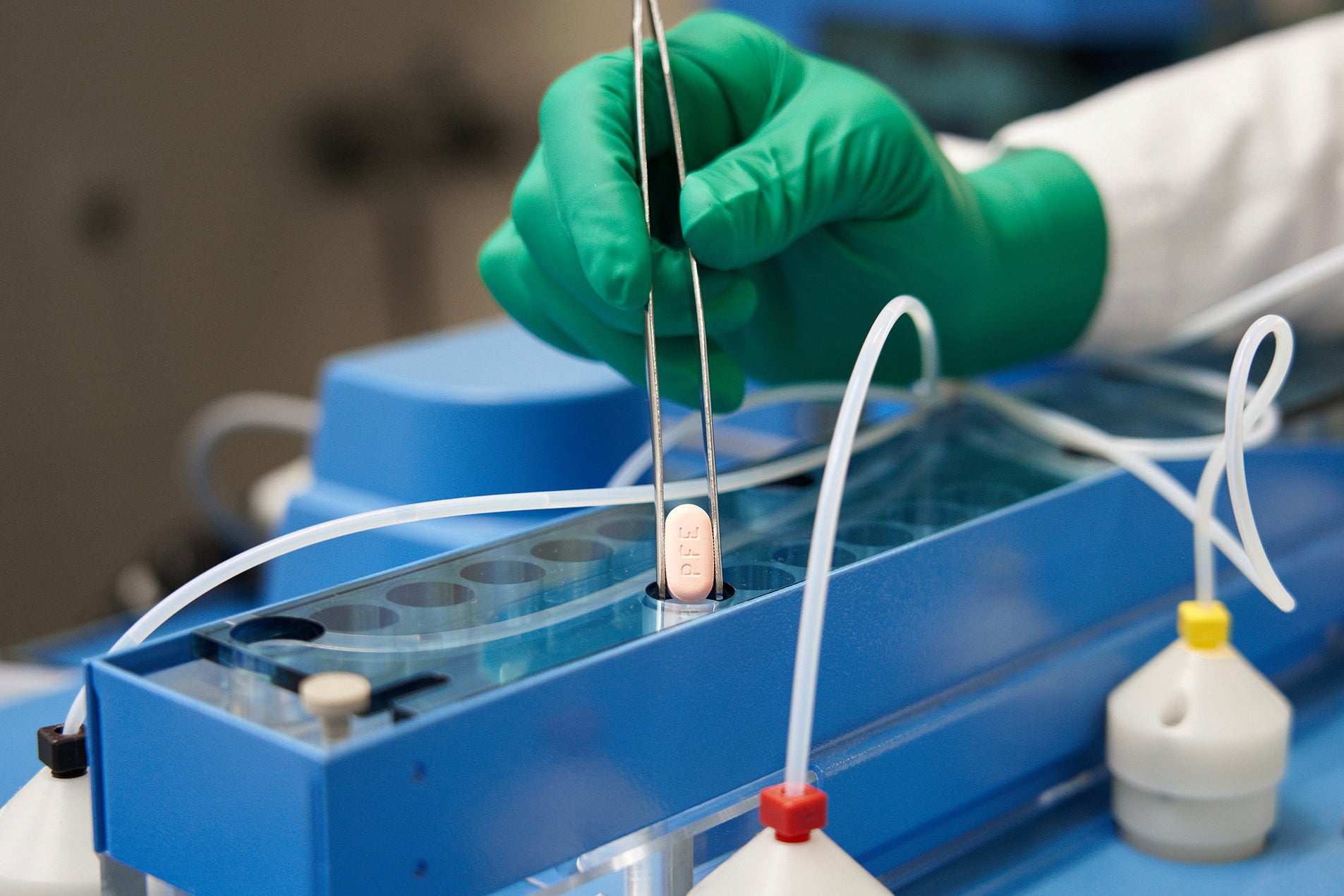
Heparin could join a string of new treatments that will be used in the UK to treat the virus. Molnupiravir, a “game-changing” antiviral drug that significantly reduces the risk of hospitalisation and death from Covid was approved for use by the UK’s medicines regulator in November while GSK’s Xevudy (sotrovimab) was also approved in December.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments