Coronavirus: Hospitals prepare for the biggest challenge of a generation
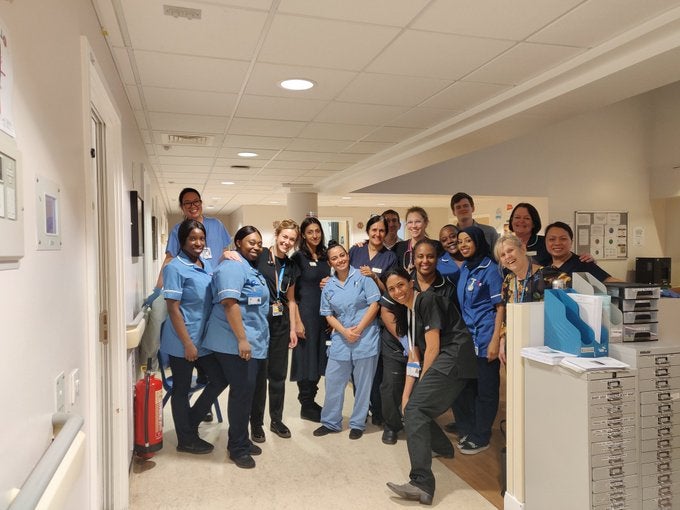
From wards popping up in a matter of days to human chains moving vital equipment, NHS staff have gone above and beyond to get ready to fight Covid-19, reports Health Correspondent Shaun Lintern


Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.It is the greatest challenge the National Health Service has ever faced. With the spectre of coronavirus looming ever larger over the UK, across the country NHS teams are working around the clock to meet the Covid-19 virus head on.
Aware they are just weeks, maybe days, from seeing a surge of critically unwell patients coming through their doors, bureaucracy has been swept to one side. The whole health service now has one singular focus – to get ready.
Walls and new wards have been refurbished and built in just days. Whole departments have been shifted to make room for coronavirus patients in hours and in every hospital the emphasis now is on everyone doing what must be done.
After a decade of austerity, bed cuts, wage freezes and staff shortages, the health service is having to dig deep to marshal the resources it needs but reports from across the UK suggest that is exactly what is happening.
There have been challenges, too, in ensuring hospitals have enough protective equipment, including face masks, with NHS England using pandemic supplies already, while at least one hospital has declared a critical incident because it had run out of intensive care beds.
The Independent has spoken to managers, doctors and nurses from across the NHS to hear how they are preparing their hospital and teams for the coming struggle.
Portakabin wards for Covid-19 patients
In many hospitals the most pressing issue is the lack of intensive care beds and respiratory support wards for patients with coronavirus who develop severe pneumonia and can struggle to breathe. In some, wards have been completely repurposed and transformed into rough-and-ready critical care units.
At the Countess of Chester Hospital, chief executive Susan Gilby said millions of pounds had been spent preparing for the virus already.
The NHS trust has created a new, second A&E department, for suspected Covid-19 patients after redeveloping an outpatient clinic and walk-in area. New walls have been built and windows removed to create a doorway into two new portable wards delivered by Portakabin in the past week.
The trust has also repurposed a portable unit into a respiratory ward in just weeks, providing 20 extra beds, as well as requisitioned offices and transformed those into a ward for patients with a total of 22 beds within days.
Ms Gilby praised her staff saying: “We have moved heaven and earth. We are not just standing back waiting for it to happen. People have worked around the clock and our estates team have been working 18 hour days, seven days a week. We are as ready as we can be.”
She said the trust now had 100 more beds available than normal and had increased its intensive care capacity fourfold since the start of the month.
A human chain
At the North Middlesex University Hospital, staff in the trust’s paediatric A&E department formed a human chain on Thursday night to move their entire department to a new location in just five hours to make space for Covid-19 patients.
Chief operating officer Andy Heeps told The Independent: “Our children’s A&E is the busiest in London, and with the population we serve, there would never be a quiet time to undertake a move such as this. But the whole of team North Mid pulled together to make it happen, and from start to finish the move was complete in just five hours.
“From the paediatric emergency medicine consultants, to nurses, to estates colleagues, IT, porters, engineers, everyone worked together to ‘lift and shift’ the paediatric A&E out of its existing space into an area that we had moved an outpatients clinic from just hours before. The energy and commitment of the team was phenomenal.”
Trust chief executive Maria Kane added: “What we’re seeing at the moment is something that is genuinely a privilege to witness, with our staff truly showing the best of public service, clinical expertise, and human kindness rolled into one.”
At Prince Charles Hospital, part of Cwm Taf Morgannwg University Health Board in Wales, two operating theatres and a recovery room were turned into intensive care wards, increasing the capacity by 200 per cent.
Consultant Dave Jones posted pictures of building work on Twitter and said: “So much activity going on, so quickly. It shows what can be achieved when everyone pulls together properly.”

At the County Durham and Darlington Foundation Trust on Friday nurses and staff worked to pack up their chemotherapy unit and move it to a community hospital all while treating patients.
Welfare packages for NHS workers
While staff across the health service work hard to prepare for the coronavirus onslaught, hospitals are also ensuring the workforce is supported. At Great Western Hospitals Trust in Swindon, bosses have created welfare packages for staff to ensure they have food, much of it donated by local pubs and hotels.
Chief executive Kevin McNamara said the trust, which also provides community care, was offering 24-hour mental health support for staff and had cancelled car parking charges.
He described the hospital now as being “unimaginable compared to what it was just a week ago” after efforts to move services and transform wards.
The trust has taken over its private patient unit to create a Covid-19 assessment unit while admin staff had volunteered to help support clinical teams.
“It would normally take a long time to make some of these decisions but the singular focus that everyone has at the moment cuts through all of that and means you can make a decision much more quickly. There has been a huge amount of effort.
“NHS staff have that sense of calling but we know that is going to be tested like it never has been tested before.”
Mr McNamara said staff had worked tirelessly but with a sense of calmness adding: “They have responded remarkably.”
He added the trust’s community teams and social care partners had played their part in helping free up hospital beds: “We have far fewer patients in hospital who didn’t to need to be there than we did 10 days ago. Everyone is pulling together; it is a real team effort.”
East Suffolk and North Essex NHS Trust has also recognised the value of looking after its staff with a staff helpline setup within 48 hours and manned from 6am to 7pm. In its first three hours the helpline took 400 calls.
Sam Allen, chief executive of the Sussex Partnership mental health trust, said she had been inundated with offers from nursing students and other clinical trainees to help care for patients. The trust has also redeployed academics and researchers back onto the frontline.
An army of volunteers
Alongside the NHS’s dedicated 1.4 million staff, the public and former health workers are stepping forward to help too. Since a public appeal went out more than 11,700 retired doctors, nurses and health professionals have signed up to be registered under emergency powers.
In addition, volunteers are being used by hospitals to help man phones, feed patients, drive vehicles and help keep the health service running by freeing up NHS workers to concentrate on key tasks.
The health secretary has described the fight against coronavirus as a “national effort” and this is no more evident then in the health service and the public response to the call to help.
Drafting in the military
While NHS trusts battle to prepare for the influx of coronavirus patients, the military has been brought in to deliver millions of face masks and protective equipment to help prevent staff getting infected.
Amid complaints the NHS was running out of equipment, NHS England said all hospitals had received a fresh delivery of equipment over the weekend. From this week, the army will help to manage and offload supplies in busy NHS settings, helping to distribute and deliver urgent supplies to the frontline with 24-hour deliveries.
The military is also planning to use east London’s Excel centre – used as a venue for the 2012 Olympics – as a potential makeshift hospital with NHS bosses discussing using the centre as a site for 500 initial patients, and potentially increasing to thousands.
London may be particularly badly hit in the coming days and The Royal London hospital, a major trauma centre and one of the busiest hospitals in the capital, is planning on spending millions of pounds refurbishing two vacant floors to create additional intensive care spaces as part of wider plans to created hundreds of new intensive care beds at the Whitechapel hospital. It normally has 22 ITU beds.
Cutting through bureaucracy
To aid the national effort the government also issued new directives on Monday giving NHS England sweeping new powers over how the NHS is structured and funded locally.
For decades the health service has been split into commissioners, who pay for services, and providers, namely hospitals, who deliver the care to patients. There are almost 200 local commissioning groups across the country.
The directions come into effect immediately and will last until the end of the year and will be used to help NHS England directly purchase 8,000 hospital beds from the private sector, at cost price, meaning 1,200 more ventilators, more than 10,000 nurses, over 700 doctors and 8,000 other clinical staff will be joining the coronavirus effort.
The biggest challenge
Chris Hopson, chief executive of NHS Providers, which represents NHS hospitals, told The Independent: “Staff across all parts of the NHS are going to extraordinary lengths and working around the clock to ensure they can safely care for their patients and also look after their own health and wellbeing.
“We have heard from our members across NHS trusts in England about the innovative ways they are creating safe areas in A&E and inpatient wards and dramatically increasing the potential capacity for patients requiring critical care, increasing the use of technology and rolling out new systems of working and shift patterns in a matter of days.
“This is by far the biggest challenge the NHS has ever faced in its history and it is striking how everyone is pulling together to prepare for the explosion in demand that is going to come.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments