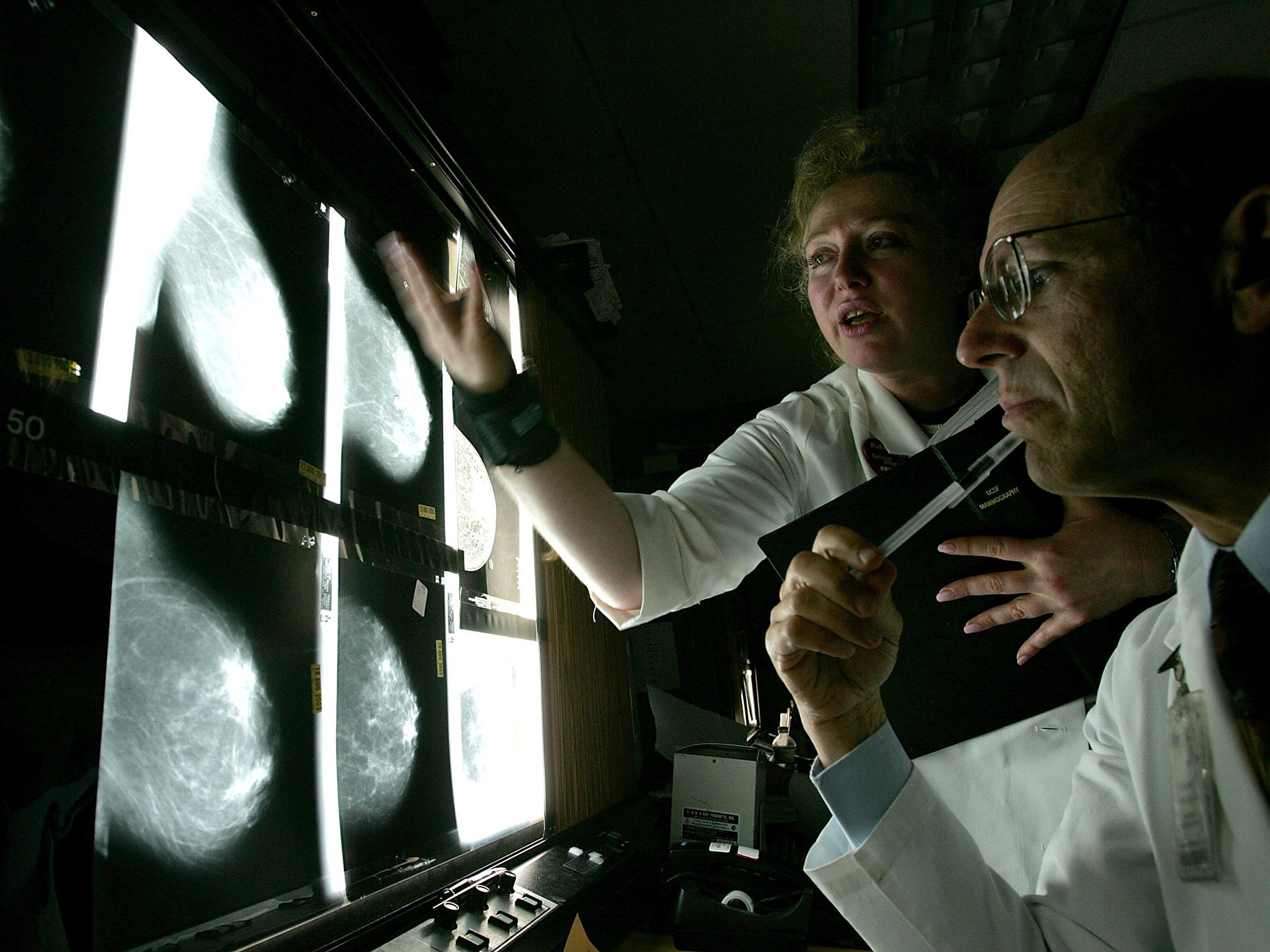
Breast cancer screening scandal could cost £100m in compensation, lawyers warn
Financial pressure in addition to demands on stretched NHS to rescan up to 309,000 women and review records of those whose care suffered from error
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Failures in breast cancer screening which the government warned may have caused hundreds of deaths and diagnosis delays could end up costing £100m in compensation, lawyers have warned.
Health and social care secretary Jeremy Hunt warned there could be as many as 270 women who died of breast cancer after missing out on their final screening invitation because of the glitch.
Clinical negligence specialists have said that the combined cost of compensating the next of kin of anyone who has died could run into the millions, but it could be even higher when factoring in other harm across all 450,000 women who missed out on tests.
“In terms of compensation we are looking at claims worth in excess of £5m plus in relation to fatal cases,” said Robert Rose, head of clinical negligence at Lime Solicitors.
“But if we factor in other damage caused to women who have survived, and the costs of legal action – if that becomes necessary – we are looking at figures of anywhere between £50-£100m.”
Mr Hunt apologised “wholeheartedly and unreservedly” this week for the error, which went unnoticed for the best part of a decade.
The NHS is writing to 309,000 women, now in their seventies, who were not called for a final checkup between age 68 and 71 to tell them of the error and invite them for a mammogram.
While he said the “best estimate” is that 135 to 270 women have died of breast cancer in this group, he said it could be substantially less, adding that the merits of national screening are “contested”.
But to begin to understand the extent of any harm, an already stretched health service will need to rapidly review the tens of thousands of women who went unscreened each year since 2009.
“The cost to the NHS in terms of doctors now having to trail through records, the cost of recalling all these women will be huge,” said Suzanne White, head of clinical negligence at law firm Leigh Day.
“I used to do mammograms – because I used to be a radiographer – they’re expensive to do, they use expensive machines and radiologists have to look at them – but there’s a shortage of radiologists.
“That’s going to cost the NHS a lot, but how you value that I don’t know.”
Ms White added this could be additional to the “£40m or £50m for compensation, and then lawyers’ fees on top”.
But she stressed that determining in each case whether the outcomes would have been better if screening had not been missed would be a very complex process.
Medical experts have said the scandal should be used to take stock of the benefits of the national screening programme, and to address a significant lack of public understanding about screening’s harms.
“I believe that the furore over the NHS breast screening programme error has resulted in unnecessary worry for those women who may not have received a breast screening invitation,” said Paul Pharoah, professor of cancer epidemiology at the University of Cambridge.
“According to the Independent UK Panel on Breast Cancer Screening report published in 2012, for every breast cancer death prevented three breast cancers will have been ‘over-diagnosed’.”
The landmark study found no improvements in overall mortality rates from screening, and women might have had very small lumps picked up – which would never become cancer – but could have led to them having unnecessary mastectomies to remove their breast or exposed them to harmful radiation treatment.
But in the wake of the announcement, the loved ones of women who died of breast cancer have said they were left devastated by the news that there was a chance their odds could have been improved.
Charities have also warned that there has been a surge in concern from women across the country.
“After this appalling blunder, Breast Cancer Care’s helpline is set to receive four times its usual number of calls by the end of the day,” said Dr Emma Pennery, clinical director at the charity.
“The women contacting us are feeling angry, confused and want answers.”
A dedicated helpline set up by Public Health England for affected women had received 8,000 calls by Thursday evening.
The Department of Health and Social Care told The Independent it was too early for it to estimate the cost of any compensation. It also could not comment on where any compensation funding would come from.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments