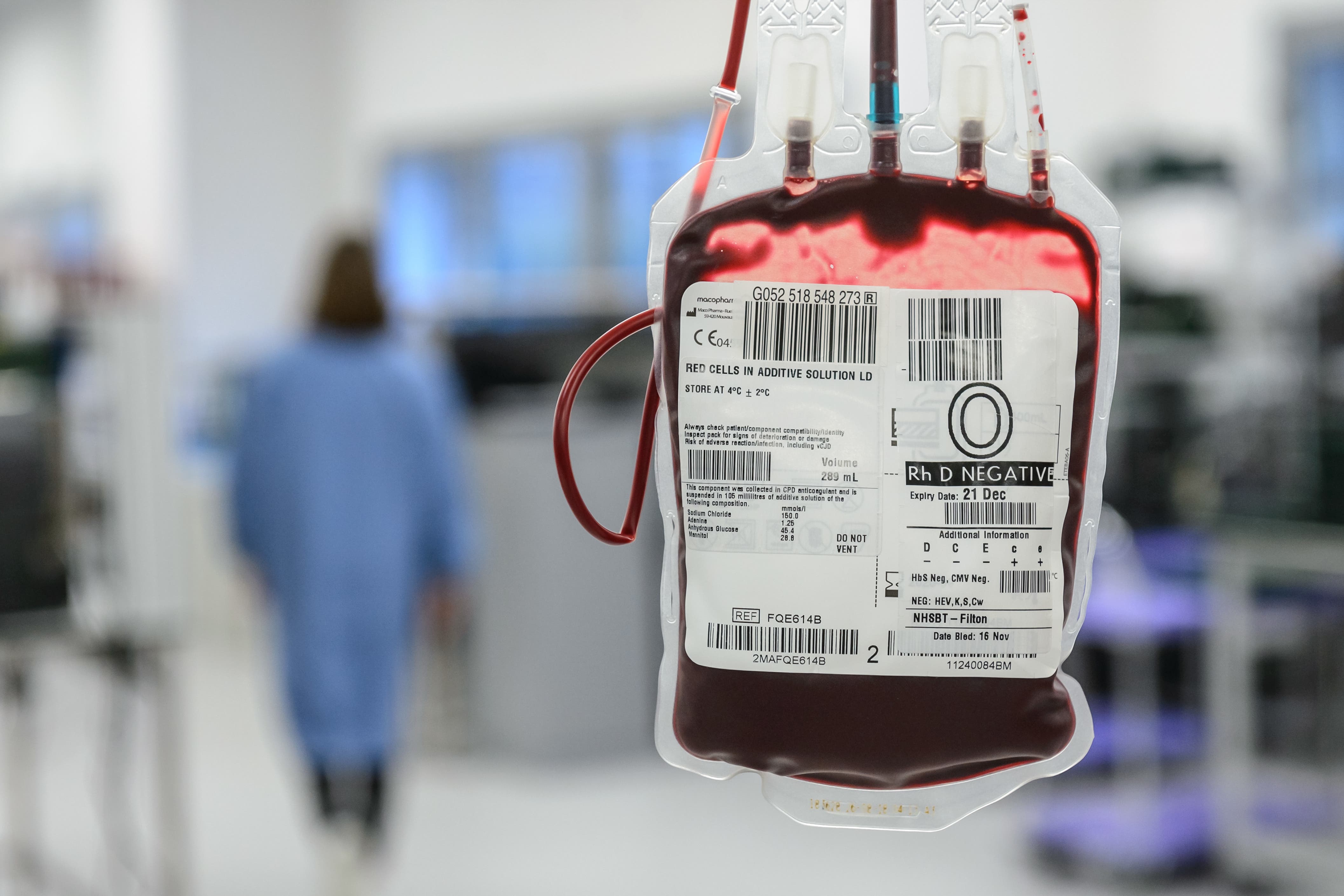
Crisis in A&E sees blood transfusion deaths up as waits and errors increase
One elderly man with an intestinal bleed died after treatment delays caused by a lack of available A&E beds
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Patients are dying from A&E blood transfusion errors as overworked staff and long waits for treatment drive up the number of safety incidents, a watchdog has warned.
Thirteen patients died in 2022 due to delays in receiving transfusions, while reports of blood errors almost doubled from 100 in 2020 to 194 last year, a new Serious Hazards of Transfusion (SHOT) report found.
The watchdog said the spike was likely driven by staffing pressures, increased workload and hospital “longer waits”.
The warning comes after the NHS’s most senior A&E doctor, Dr Adrian Boyle, told The Independent that thousands of patients could needlessly die this winter because of the government’s failure to plan for enough emergency staff and beds.
As the A&E crisis deepens, the government confirmed on Tuesday that the NHS would get £250m to fund 900 extra beds to cope with winter pressures. But health leaders have warned this will only make a difference if staffing is also boosted.
The SHOT report found “staffing challenges” and “poorly resourced systems” were leading to preventable errors with transfusions. It found emergency departments were often “very busy” and the number of overall errors reported in A&Es “continues to increase”.
It added: “Problems with staffing and workload were identified in many reports. Responses to human factors questions from reporters have highlighted issues relating to a mismatch between staffing and workload, as well as poor communication.”
Patient deaths due to blood transfusion delays rose to 13 in 2022, up from 12 in 2020, nine in 2019 and just two in 2018. And the number of delays in patients receiving blood increased to 205 in 2022, up from 129 in 2021.
One elderly man with a gastro-intestinal bleed who attended A&E during a bank holiday died after treatment delays caused by a lack of beds. The report found nurses had attempted to escalate his deterioration to doctors but the medical team was “stretched, having to review patients across multiple wards”.
Another man, in his 70s, arrived at A&E with chest pain and confusion having been discharged with Covid two days earlier. The man, who was on warfarin blood thinner tablets and was covered in bruises, was found unresponsive and later died after a 12-hour wait for treatment.
The incident report noted “an overcrowded department will have contributed to staff fatigue, stress and distraction with a consequent negative impact on cognitive biases”.
In a third report, of a 60-year-old man who did not receive the blood transfusion he needed, reviewers said staffing issues had since led to a nurse quitting her job.
“There were only two qualified nurses on duty overnight with a full ward and four patients who were actively bleeding. The nurse was exhausted and had to take time off work. She was a very experienced nurse but following a period of sick leave and counselling, she has resigned from her post,” the report said.
Staff shortages within blood labs were also noted as a common driver of incidents, with the report warning the issue “must be addressed urgently”.
It added: “Adequate numbers of appropriately trained staff must be available to ensure safe transfusions; there should be contingency planning for staffing levels below a minimum level and for times of high workload.”
Dr Boyle, president of the Royal College of Emergency Medicine, told The Independent the report’s findings were “another indicator of the pressure that our emergency departments are under”.
He said: “Reducing the serious harms from maladministration of blood products is complex, with many moving parts. Retaining experienced staff, providing adequate training and quality assurance and creating a calm enough environment so that overwhelmed staff aren’t distracted while performing safety-critical interventions would clearly help.”
Earlier this year, The Independent revealed that 50,000 patients a week were left waiting more than 12 hours in A&E during the height of the winter crisis in December.


Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
0Comments