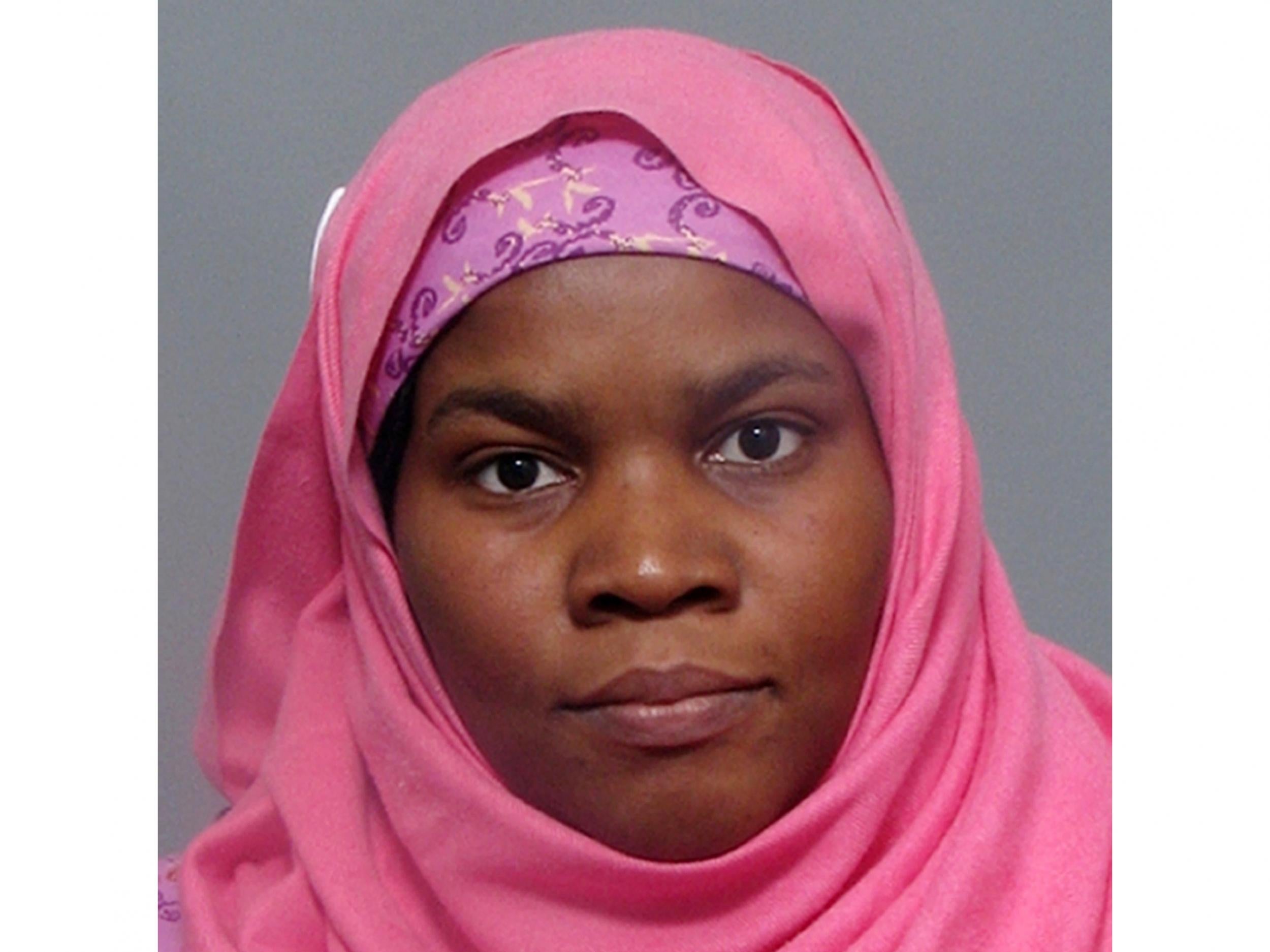
Hadiza Bawa-Garba: Medics raise £200,000 legal fund for junior doctor struck off over six-year-old's death
Decision to push for Dr Bawa-Garba to be stripped of her medical licence following mistakes in under pressure hospital has wide-ranging impact for NHS, doctors warn
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Doctors have raised £200,000 for legal support of a trainee paediatrician Dr Hadiza Bawa-Garba who was stripped of her licence to practise medicine following the death of six-year-old Jack Adcock.
The target has been hit with 27 days remaining and will be used to fund an independent legal team to review her case and potentially challenge the original ruling of causing manslaughter by gross negligence.
Funds raised can only be spent on legal fees, and the doctors behind the campaign warn that taking the case forward has to consider the “enormous cost liabilities” that she could incur if the subsequent appeal is lost.
Thousands of doctors have also signed a letter warning there will be wide-ranging consequences from the ruling which they say will make doctors working in the overstretched NHS more risk-averse and less likely to admit mistakes.
The letter supports the need to be transparent about mistakes and learn from them, as in the case of Jack Adcock’s death from sepsis.
But it adds: “As fellow doctors we have deep-seated concerns about the implications that follow from Dr Bawa-Garba’s manslaughter conviction and striking from the medical registrar.”

The case against Dr Bawa-Garba used evidence from personal appraisals, which doctors are required to maintain and use for learning and reflection, in the case against her.
This is another major concern for doctors who are taking to social media to say in future they will only reflect in one-to-one discussion with their appraiser, and will no longer write down anything that could be used against them.
It is a worry shared by Health and Social Care Secretary Jeremy Hunt, who tweeted last week that the action of the GMC will prevent the NHS from learning lessons when things go wrong.
Mr Hunt has staked his legacy on making the NHS more transparent and has said he wants to instil a no-blame culture akin to the airline industry.
The GMC case was brought against the decision of its own Medical Practitioners Tribunal Service, which said Dr Bawa-Garba should be allowed to return to work after a 12-month suspension.
The MPTS takes a fuller picture of the medical context and decisions in each case, but the GMC said its decision was “not sufficient” to protect the public or maintain confidence in the medical profession.
On Thursday, the UK High Court upheld the GMC’s appeal and call for Dr Bawa-Garba’s “erasure” from the medical register for the mistakes which led to Jack Adcock’s death and saw her handed a two-year suspended jail sentence.
But doctors warn that the initial court ruling and subsequent High Court case failed to look at medical realities, including the exceptional pressures and system-wide failings that led to the six-year-old’s death in February 2011.
At the time, Dr Bawa-Garba was a specialist registrar in her sixth year of training to be a paediatrician, working at Leicester Royal Infirmary.
She had recently returned from maternity leave and because there was no senior consultant available she was solely in charge of the emergency department and acute Children’s Assessment Unit.
There was also an IT failure which led to delays in obtaining test results.
Dr Bawa-Garba did make mistakes, including failing to ask a consultant to review Jack’s condition and confusing him with another patient and briefly stopping CPR (though this latter case was not deemed to have contributed to his death).
However many doctors have shared cases of similar failings, and warn they will have only become more common as NHS funding and staff shortages have worn on over the last eight years.
Responding to the campaign in a statement, the paediatrician said: “I share all of your concerns about the implications of this case and the General Medical Council’s (GMC) actions on future patient safety.
“In the light of this huge outpouring of support, I plan to use your generous funds to change to a top independent legal team, to potentially challenge the GMC and to have an independent review of the original conviction.
“I am truly humbled by what you have done for me.”
Dr James Haddock, Dr Moosa Qureshi and Dr Chris Day, who started the crowdfunding push said: “Please continue to donate generously.
“CrowdJustice money can only be spent on legal fees, and your donations will make a significant difference to how much Hadiza can achieve.
“The more we raise, the more her team can do. There are tremendously serious legal and healthcare issues raised by Hadiza’s case which will affect all healthcare professionals and patient safety as the NHS is increasingly put under stress.”
After the High Court ruling last week, GMC chief executive Charlie Massey said tribunals cannot circumvent a decision by a court jury, adding: “This has been a tragic case; a family has lost their son in terrible circumstances and a doctor has lost her career.
“In today’s ruling the court has confirmed that the Tribunal was simply wrong to conclude that public confidence in the profession could be maintained without removing the doctor from the medical register.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments