California virus surge brings body bags, makeshift morgues
California is distributing 5,000 body bags mostly to the hard-hit Los Angeles and San Diego areas and has 60 refrigerated trailers standing by as makeshift morgues in anticipation of a surge of coronavirus deaths
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.California is distributing 5,000 body bags mostly to the hard-hit Los Angeles and San Diego areas and has 60 refrigerated trailers standing by as makeshift morgues in anticipation of a surge of coronavirus deaths from hospitalizations that now are double the summertime peak and threaten to overwhelm the hospital system, Gov. Gavin Newsom said Tuesday.
The number of average daily deaths has quadrupled from 41 a month ago to 163 now, while positive cases have surged to more than 32,500 each day. Of those new cases, an anticipated 12% will wind up in the hospital and 12% of those hospitalized will crowd already stretched intensive care units.
That means one day's worth of cases can be expected to produce a staggering 3,900 hospitalizations and nearly 500 ICU patients.
“We are in the middle of the most acute peak,” Newsom said, urging residents to take precautions to slow the spread.
In Southern California’s Orange County, health officials said mobile field hospitals would be rolled out to three hospitals that already need more space. The large, heavy-duty, temperature-controlled canvas tents with hard flooring add an extra 125 beds.
Dr. Clayton Chau, the county’s public health officer. told the county’s Board of Supervisors that “emergency rooms have no capacity to triage people as quick as they can." He pleaded with residents to avoid gathering with people from outside their households.
“I have never been so afraid of Christmas and New Year’s in my life,” Chau said. “I can’t imagine what it would be like after the holidays if people are not listening.”
At the meeting where Chau spoke, dozens of residents didn't wear masks and demanded businesses be allowed to reopen.
To the north, Santa Barbara County Public Health Director Van Do-Reynoso said in a statement the county is “reaching a point where we can see on the horizon our health care system being overrun. We must take immediate action as our decisions are now seeing the price to be paid, and it is costing the lives and wellbeing of our community members.”
The surge in cases throughout much of California is forcing an urgent scramble for more staff and space, a crush that Newsom and the state’s top health official said might not abate for two months despite the arrival of the first doses of vaccines this week.
The surge already has prompted an easing of normal nurse-to-patient ICU ratios and quarantine standards for health care workers, and the opening of more alternative care facilities. State officials are reaching out to the Department of Defense and overseas staffing services for desperately needed medical workers.
The California Nurses Association denounced reducing the ratio of ICU nursing care, saying in a statement that it “will inevitably lead to more patient, nurse, and other health care worker infections and deaths."
Newsom said it is part of “a very dynamic effort” to get more staffing, particularly in intensive care units.
Newsom announced a new shutdown order nearly two weeks ago that is based on ICU capacity. Nearly the entire state now is under the most severe restrictions.
California has brought in 507 extra staff and deployed them around the state, though most don't have the skills to help in ICUs. The state is seeking a total of 3,000 contracted medical staff.
“Two weeks from now we are concerned about what our ability to provide the same level of high quality care will be,” said Dr. Mark Ghaly, California’s secretary of health and human services. He said hospitals have been planning for the worst, including updating what are called “crisis care guidelines” in case they must start triaging which patients get what level of treatment.
“Hospitals are in a very challenged situation right now,” said Carmela Coyle, president and CEO of the California Hospital Association. “That will only get worse, and potentially far worse in the next 30 days or so."
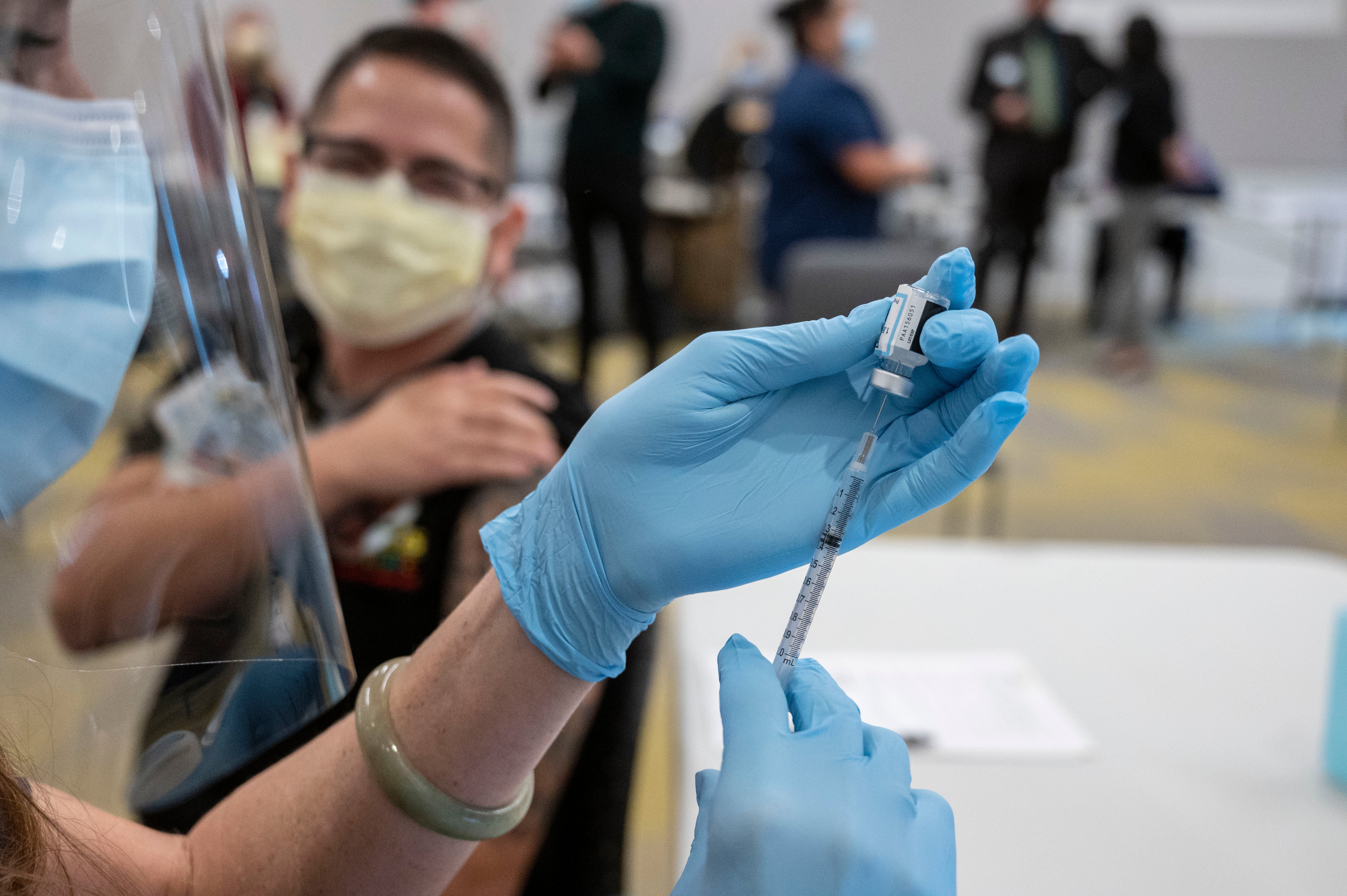
In a rare bit of good news, Newsom said that nearly 394,000 more doses of Pfizer vaccines could arrive in California next week on top of the nearly 328,000 doses being distributed at 33 locations this week.
Even the joyful first inoculations at one of Northern California’s biggest hospitals were tinged with sadness Tuesday.
Eva Teniola, 47, a clinical nurse in the University of California, Davis Medical Center’s emergency department for the last 10 years, called it the “hero vaccine” as she spread her arms wide upon becoming the hospital’s first employee to receive the vaccine. She said she’s never seen anything as bad as the coronavirus, which has forced people to die without their families by their sides.
“These past few weeks, it’s really different,” she said, adding that she can see the toll on her colleagues’ faces. “It’s like burnout. We get tired, you know ... the pressure, the stress.”
For Shashi Kant, a senior custodian in the hospital’s ICU, getting the vaccine was even more personal. His adult daughter, a radiology technician at a Modesto hospital, died from the virus several months ago.
“This is just like a lifeline,” he said about getting the vaccine. “I’m protecting myself and the patient.”
Protecting health care workers with the first vaccines could help hospitals deal with the surge because they won't lose so many workers to quarantines or the illness, said health policy professor Joanne Spetz, the associate director of research at the Healthforce Center at the University of California, San Francisco.
The health care system has also made strides in learning new treatments and ways to divert some patients from needing the most intensive care. Yet she said in an interview that all those may come into play now particularly if cases surge even higher with the holidays.
“People who land in the ICU with COVID are just really, really sick and can be there for quite a long time,” she said. "So I think that adds to the alarm bells around this and the concern about the potential overwhelming of the facilities.”
___
Associated Press writers John Antczak in Los Angeles, Amy Taxin in Orange County and Kathleen Ronayne in Sacramento contributed to this story.