More same-sex couples and single parents using IVF to start families, figures show
Success rates of IVF are also continuing to improve
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.More same-sex couples, single women and surrogates are using in vitro fertilisation (IVF) treatment, news figures show.
According to the Human Fertilisation and Embryology Authority (HFEA) – the UK’s independent regulator of fertility treatment and research using human embryo – more than 54,000 patients underwent around 75,000 fertility treatments in 2017.
The data, which relates to treatment cycles carried out in 2017, shows that IVF treatment cycles have also increased by 2.5 per cent since 2016, resulting in over 20,500 babies being born.
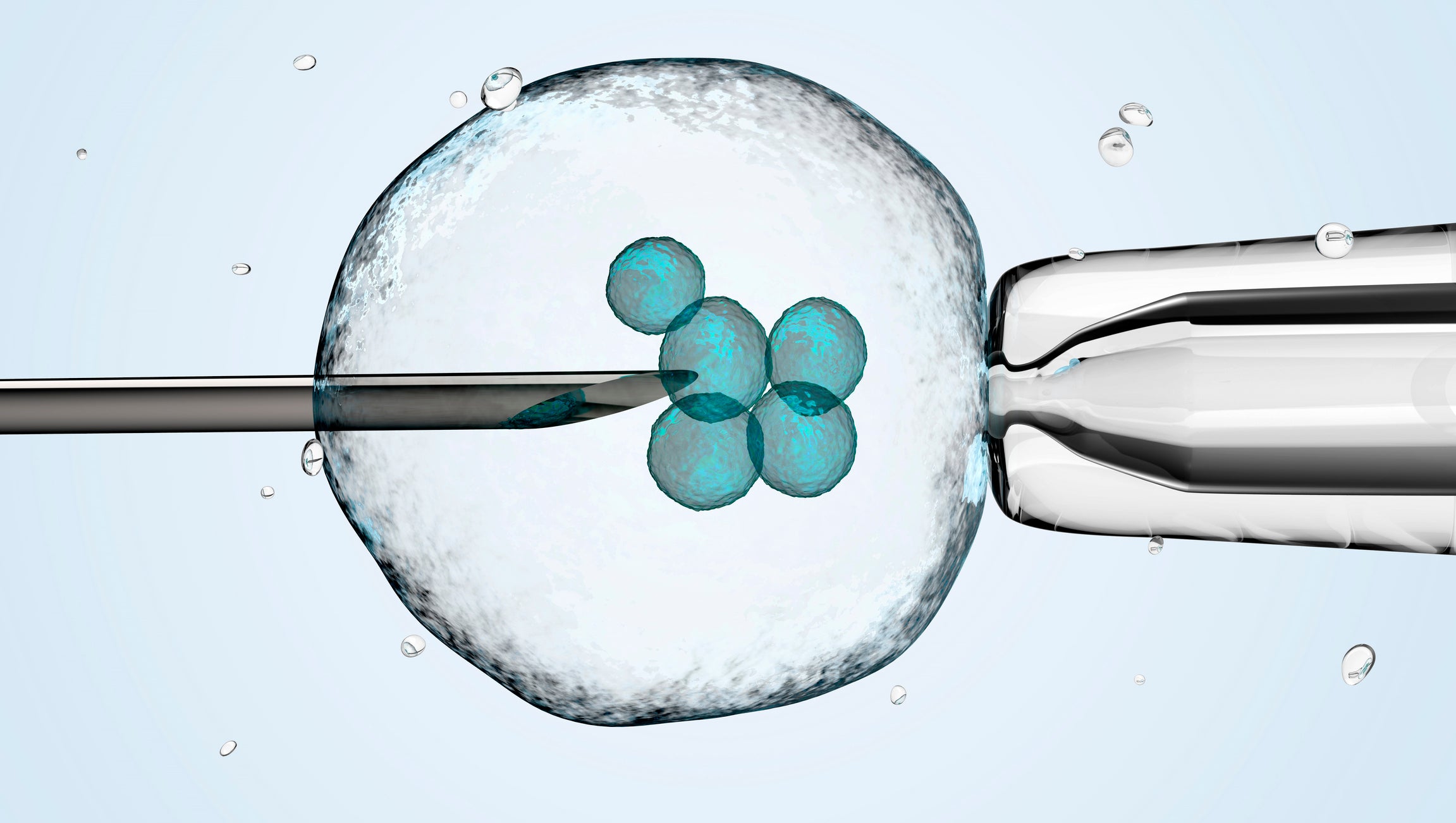
IVF is one of several techniques available to help people with fertility problems have a baby, the NHS states.
During IVF, an egg is removed from the woman's ovaries and fertilised with sperm in a laboratory. The embryo is then returned to the woman's womb to grow and develop.
Success rates of IVF are also continuing to improve, with the average birth rate for women using their own eggs reaching 22 per cent.
Women aged under 35 using their own eggs are found to have the highest birth rates with 30 per cent for a fresh cycle and 27 per cent for a frozen cycle.

The report also indicates that IVF is becoming safer as fewer patients are having twins.
The figures show that multiple births, which is the single biggest health risk from IVF, has reached an all-time low of 10 per cent, marking a sharp decline from 24 per cent in 2008.
Speaking about the findings, Sally Cheshire CBE, Chair of the Human Fertilisation and Embryology Authority, said: “Fertility treatment has come a long way over more than 40 years and is now safer whilst helping more people to create their much longed for families.
“We know that multiple births carry higher risks to mothers and babies and cost more to the NHS. That’s why, it is a great achievement that all our hard work with fertility clinics has paid off as we have now achieved the lowest ever multiple birth rate while continuing to see success rates rise.”
The average age of patients undergoing both IVF and donor insemination (DI) treatments has increased from 33.5 and 32 in 1991 to 35.5 and 34.5 in 2017, respectively.
The majority (90.7 per cent) of treatment cycles in 2017 were undertaken by patients with male partners. The remaining patients were listed with a female partner (5.9 per cent), no partner (3 per cent) or as a surrogate (0.4 per cent).
However, the fastest growing fertility treatment type is egg freezing, which has increased by 11 per cent since 2016 to 1,462 cycles in 2017.
Frozen cycles success rates at 23 per cent have overtaken those of fresh embryo cycles (21 per cent) for the first time since records began.
As for a UK breakdown of treatments, 62 per cent of treatment cycles are NHS-funded in Scotland and 50 per cent in Northern Ireland.
Meanwhile only 39 per cent and 35 per cent are NHS-funded in Wales and England.
Prof Allan Pacey, Professor of Andrology, University of Sheffield, describes the nationwide funding discrepancies as “alarming”.
“What is alarming to me is the shocking difference in NHS funded cycles across the four nations of the UK, with Scotland being the most generous and England being the least,” he says.
“This is really shameful and unfair. We really need to change this and make NHS provision of IVF equitable, regardless of where people live.”
Prof Joyce Harper, Professor in Human Genetics and Embryology, University College London (UCL), concurred, adding: “Fertility treatment is turning into a middle class procedure, with the UK having some of the highest IVF costs in Europe. It is time to address the commercialisation of IVF and how the NHS fund it.”
The National Institute for Health and Care Excellence (NICE) fertility guidelines make recommendations about who should have access to IVF treatment on the NHS in England and Wales, the NHS states.
Under NICE’s guidelines, it is recommended that IVF should be offered to women under the age of 43 who have been trying to get pregnant through regular unprotected sex for two years, or who have had 12 cycles of artificial insemination.
However, the final decision about who is able to receive NHS-funded IVF in England is made by local clinical commissioning groups (CCGs).
Earlier this year, a study the Royal College of Obstetricians and Gynaecologists (RCOG), found that almost half of young women would consider freezing their eggs in future.
According to the research, 25 per cent of women aged between 18 and 24 are worried about their ability to conceive, a concern also shared more widely by 49 per cent of women of all ages in the UK.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments