Gene correction technique could revolutionise treatment
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Scientists have performed a “seamless” correction to a faulty gene behind an inherited form of anaemia using a revolutionary new technique in genome editing that could transform the treatment of many genetic diseases.
Two mutations in the haemoglobin gene of a patient with beta thalassemia – which can cause severe anaemia – were corrected without any errors using the Crispr technique of genome editing, the researchers said.
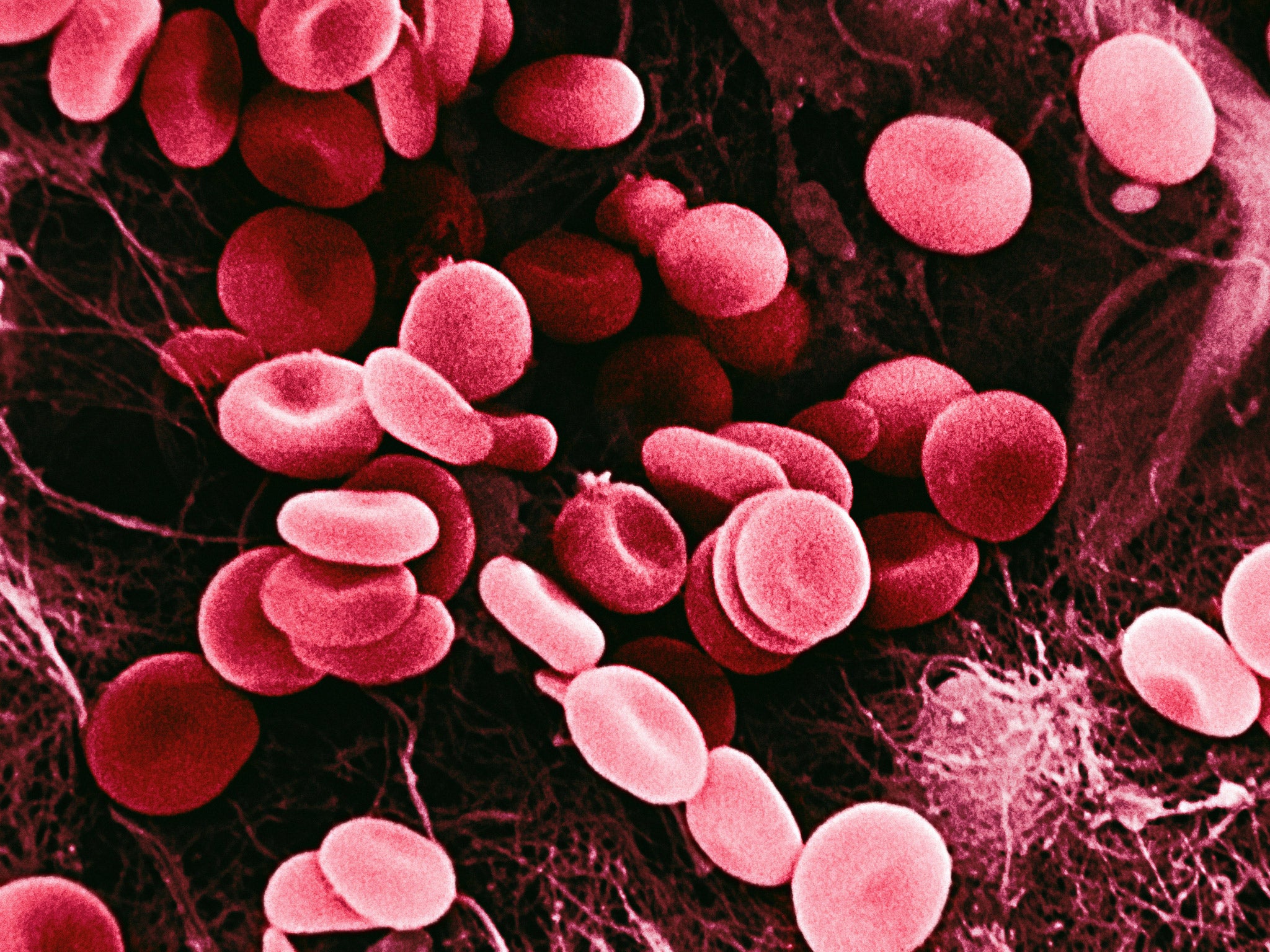
The experiment involved converting the patient’s skin cells into stem cells in the laboratory so that the faulty gene could be corrected before the stem cells were allowed to mature into red blood cells. Without the genome correction, the red cells would have become deformed and sickle-shaped as a result of the defective haemoglobin gene.
Crispr is a new way of editing the human genome with extreme accuracy and efficiency, and has generated intense interest across the world since it emerged last year. In this study it corrected the two inherited mutations of a Chinese patient’s haemoglobin gene with perfect precision, the scientists said.
However, although the Crispr editing produced healthy red blood cells in laboratory dishes, the researchers did not transfuse them back into the patient – a critical step that would require further research as well as ethical approval, they said.
Yuet Wai Kan of the University of California, San Francisco, the lead author of the study published in the journal Genome Research, said: “I believe it will take quite a few more years before we can apply it in a clinical setting.”
Patients with severe forms of beta thalassemia need blood transfusions repeatedly and often suffer complications to their spleens, livers, hearts and bones. Being able to produce healthy red blood cells from the patients themselves could lead to better treatments or even a one-off cure.
Professor Kan said that Crispr corrected the patient’s faulty haemoglobin gene “seamlessly and efficiently”, marking an important step towards effective gene therapy for thalassemia patients.
“Our laboratory has been studying sickle cell disease and thalassemia for many years and developed DNA tests for them in the 1970s,” Professor Kan said.
“In recent years, we turned our research to explore their treatment through stem cell therapy by correction of the mutations in the patient’s own cells,” he said.
The first stage of the study involved transforming the patient’s skin cells into an embryo-like state using a technique called induced pluripotent stem cells (iPS). After this stage, the scientists used the Crispr technique to correct the double fault in the patient’s gene for the beta protein of the haemoglobin molecule, which carries oxygen in the bloodstream.
The scientists were able to remove all the genetic “markers” used in the procedure so that the resulting red blood cells showed no evidence of having any corrections made to its DNA – they were also healthy in appearance and shape.
However, a major hurdle to using the technique in clinics is to find a way of producing enough high-quality red blood cells that can be transfused back into the patient, Professor Kan said.
“Although we and others are able to differentiate iPSCs into blood cell progenitors as well as mature red blood cells, the transplantation of progenitors into mouse models to test them has so far proven very difficult,” Professor Kan said.
Beta thalassemia is more common among people from countries with a recent history of malaria, such as Greece, Cyprus, Italy, the Middle East and sub-Saharan Africa, and is thought to confer a slight advantage in surviving the disease.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments