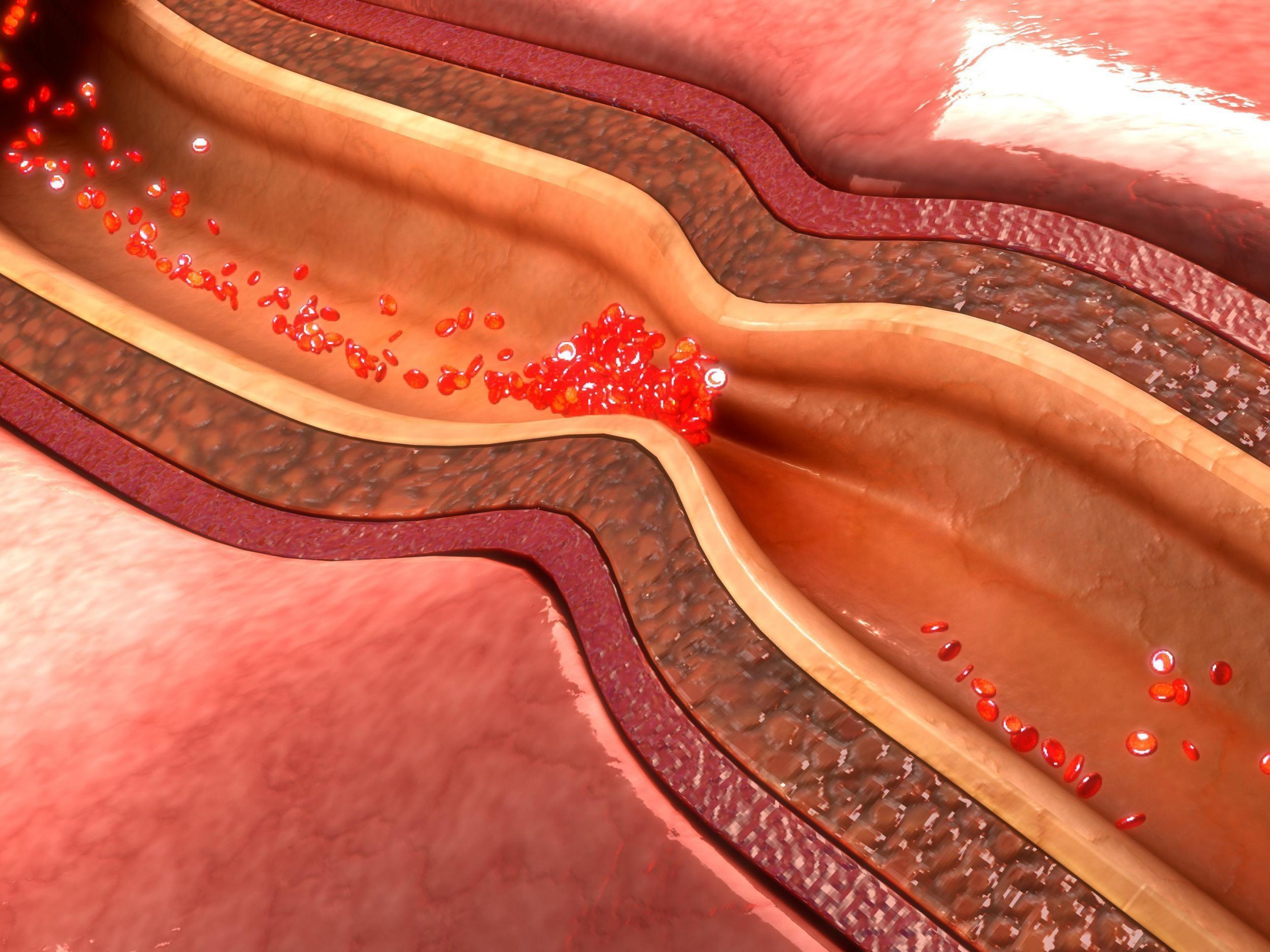
Depression doubles the risk of death from coronary artery disease, finds research
While depression seems to make the condition worse, being diagnosed is also a reason why some patients become depressed
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Depression appears to double the chance of dying in any given year for patients with coronary artery disease, according to a new study.
The researchers said such mental distress was a “stronger risk factor” than age, having had a heart attack, or diabetes.
The effect was seen if the person was depressed before or after diagnosis of the disease.
Nearly 25,000 people with coronary artery disease were tracked over an average of 10 years and about 15 per cent of them ended up being diagnosed with depression, according to a paper published in the European Heart Journal.
Dr Heidi May, a cardiovascular epidemiologist at Intermountain Medical Centre Heart Institute in Salt Lake City, said: “No matter how long or how short it was, patients were found to have twice the risk of dying compared to those who didn’t have a follow-up diagnosis of depression.
“Depression was the strongest risk factor for dying, compared to any other risk factors we evaluated. That included age, heart failure, diabetes, high blood pressure, kidney failure, or having a heart attack or stroke.
“We’ve completed several depression-related studies and been looking at this connection for many years.
“The data just keeps building on itself, showing that if you have heart disease and depression and it’s not appropriately treated in a timely fashion, it’s not a good thing for your long-term wellbeing.”
Of more than 2,600 patients who became clinically depressed about 27 per cent did so within a year of being diagnosed with the disease. The figure was 37 per cent after five years.
And while depression seems to make the condition worse, being diagnosed is also a reason why some patients become depressed.
The reason why the chance of dying increased was not revealed by the study, but Dr May said it was possible patients were not following their treatment plans as closely as people in good mental health.
“We know people with depression tend to be less compliant with medication on average and probably in general aren’t following healthier diets or exercise regimens,” she said.
“They tend to do a poorer job of doing things that are prescribed than people without depression. That certainly doesn’t mean you’re depressed so you’re going to be less compliant, but in general, they tend to follow those behaviours.”
She added that depression can also cause physiological changes to the body, which could also be a factor.
Dr May urged the medical community to take depression seriously when treating coronary artery disease.
“Patients who have depression need to be treated to improve not only their long-term risks but their quality of life,” she said.
“I hope the takeaway is this: it doesn’t matter how long it’s been since the patient was diagnosed with coronary artery disease. Continued screening for depression needs to occur.
“After one year, it doesn’t mean they’re out of the woods. It should be ongoing, just like we keep measuring things like LDL cholesterol.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments