Breakthrough in human cloning raises hopes for treatment of Parkinson's and heart disease
News could lead to tissue-transplant operations for range of debilitating disorders, also including MS and spinal cord injuries
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Scientists have finally made the long-awaited breakthrough in human cloning by turning skin cells into early-stage embryos that were then used to create specialised tissue cells for transplant operations, it has been revealed today.
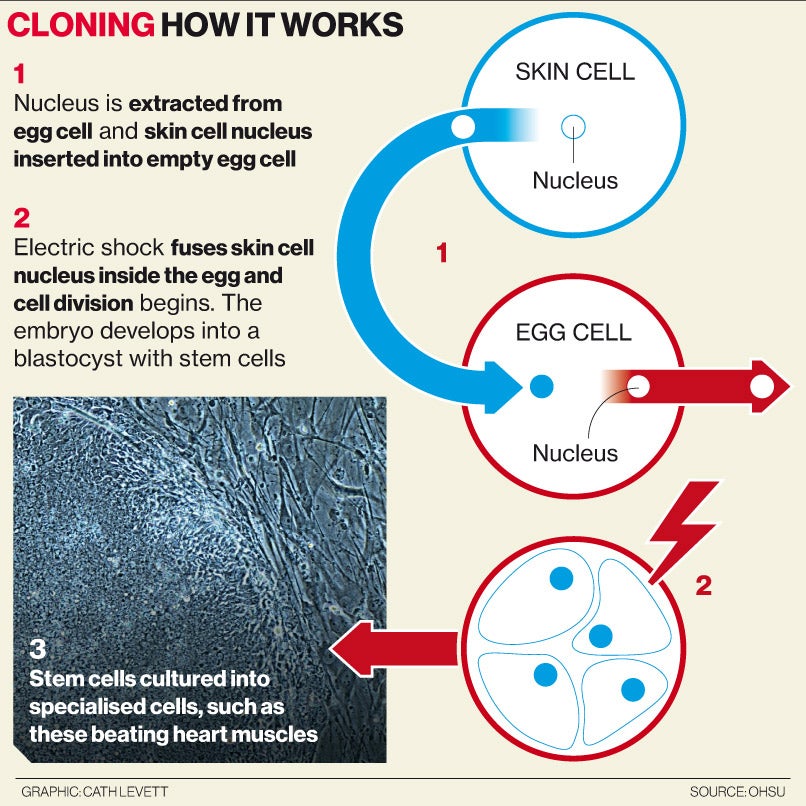
For the first time, researchers have unequivocally created human embryonic stem cells using the cloning technique that led to the birth of Dolly the sheep. However, unlike Dolly, the human embryos were destroyed when their stem cells were extracted.
The scientific milestone, which comes 17 years after the birth of Dolly, represents a major turning point in human cloning research which could now lead to new tissue-transplant operations for a range of debilitating disorders, such as Parkinson's disease, multiple sclerosis, heart disease and spinal cord injuries.
However, the breakthrough will also raise serious ethical concerns about the creation of human embryos for medical purposes and the possible use of the same technique to produce IVF embryos for couples wanting their own cloned babies - which is currently illegal in the UK.
The scientists who made the advance emphasised that the work is designed to produce replacement tissue for transplant operations from a patient's own skin cells, rather than to improve the chances of so-called “reproductive cloning”. However, other scientists said the achievement inevitably brings the prospect of cloned babies a step nearer.
Generating a plentiful supply of embryonic stem cells from a patient's own skin cells has been one of the holy grails of medical science. Although the procedure has been achieved in laboratory animals - such as mice and monkeys - it has until now alluded several attempts on human material.
Shoukhrat Mitalipov, who led the research team at the Oregon Health and Science University in Portland, said that he added caffeine to his cell cultures to create viable embryonic stem cells from just a small number of human eggs.
“It was thought that to make [it] work many thousands of human eggs would be needed. We were able to produce one embryonic stem cell line using just two human eggs which would make this approach practical for widespread therapeutic use,” Dr Mitalipov said.
“Our finding offers new ways of generating stem cells for patients with dysfunctional or damaged tissues or organs. Such stem cells can regenerate and replace those damaged cells and tissues and alleviate diseases that affect millions of people,” he said.
In 2004, scientists led by the disgraced Woo Suk Hwang of Seoul National University claimed to have produced the first cloned human embryos, and later said they had extracted embryonic stem cells, but they were forced to retract the research after a scandal over fraudulent results and unethical practices.
Other researchers also claimed to have produced cloned human embryos but none had been able to show definitively that they could generate plentiful supplies of embryonic stem cells that could be converted in the laboratory into fully specialised tissue cells, such as beating heart muscle.
Dr Mitalipov made important technical advances that enabled the cloned human embryos to survive to the 150-cell stage, known as a blastocyst, when embryonic stem cells can be extracted for growing in the laboratory into specialised tissue cells, such as nerve cells or cardiac muscle.
“A thorough examination of the stem cells derived through this technique demonstrated their ability to convert just like normal embryonic stem cells, into several different cell types, including nerve cells, liver cells and heart cells,” Dr Mitalipov said.
“Furthermore, because these reprogrammed cells can be generated with nuclear genetic material from a patient, there is no concern of transplant rejection. While there is much work to be done in developing safe and effective stem-cell treatments, we believe this is a significant step forward in developing cells that could be used in regenerative medicine,” he said.
The research was directly aimed at generating embryonic stem cells for treating serious disorders from a patient's skin cells, and not at improving the chances of producing cloned babies, Dr Mitalipov said.
“This is not our focus, nor do we believe our findings might be used by others to advance the possibility of human reproductive cloning,” he said.
However, David King director of the pressure group Human Genetics Alert, said: “Scientists have finally delivered the baby that would-be human cloners have been waiting for: a method for reliably creating cloned human embryos. This makes it imperative that we create an international legal ban on human cloning before any more research like this takes place. It is irresponsible in the extreme to have published this research.”
Paul De Sousa of Edinburgh University said the breakthrough means a technique that was once considered impractical could now be used to generate plentiful supplies of human embryonic stem cells for future transplant operations.
“They have shown it to be a very efficient procedure based on a relatively small number of eggs. It indicates that the procedure is clinically transferable. It's an important step,” Dr De Sousa said.
Professor Mary Herbert of Newcastle University, said: “Provided that the experiments are reproducible in the hands of others, the findings offer the potential to accelerate progress towards the development of patient-specific embryonic stem cells to treat a range of degenerative diseases.”
The study is published in the journal Cell.
Watch videos on the steam research below:
Animation of stem cell reprogramming process
Animation of stem cell reprogramming process from OHSU Video on Vimeo.
Beating heart cells
Video of beating heart cells from stem cells derived from skin cells from OHSU Video on Vimeo.
Dr Shoukhrat Mitalipov explains the research
Sound bites from Dr. Shoukhrat Mitalipov, Ph.D. from OHSU Video on Vimeo.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments