New research confirms a link between autoimmune disorders and psychosis
The study found the likelihood of having psychosis was higher for disorders like pernicious anaemia, psoriasis and coeliac disease
People with autoimmune disorders, a collection of diseases where the body’s immune system attacks its own cells, are more likely to develop psychosis, according to our latest research.
Previous research found that rates of rheumatoid arthritis were lower in people with psychosis than would be expected in the general population. But later studies showed that other autoimmune disorders, such as coeliac disease and autoimmune thyroid disorders, were more common in people with psychosis.
This led scientists to the view that there is a connection between autoimmune disorders and psychosis. But conflicting findings meant that it was difficult to reach any conclusions about the relationship.
Given the uncertainty about the relationship between these disorders and psychosis, and growing interest in this area, we decided to review the research and conduct a meta-analysis – a method in which data from several studies are combined and analysed together to give a more statistically robust result than individual studies can provide.
Our study, which is published in Biological Psychiatry, included 30 relevant studies, and contained data on 25 million people.
We focused on autoimmune disorders that affect the peripheral system, such as type 1 diabetes, as we were particularly interested in whether autoimmune disorders that target the body, as opposed to the brain, could still influence the development of psychosis.
For our main analysis, we combined data from all non-neurological autoimmune disorders, except for rheumatoid arthritis (given the well-established negative association reported with psychosis) and found that, overall, people with any autoimmune disorder were 40 per cent more likely to have a psychotic disorder, such as schizophrenia.

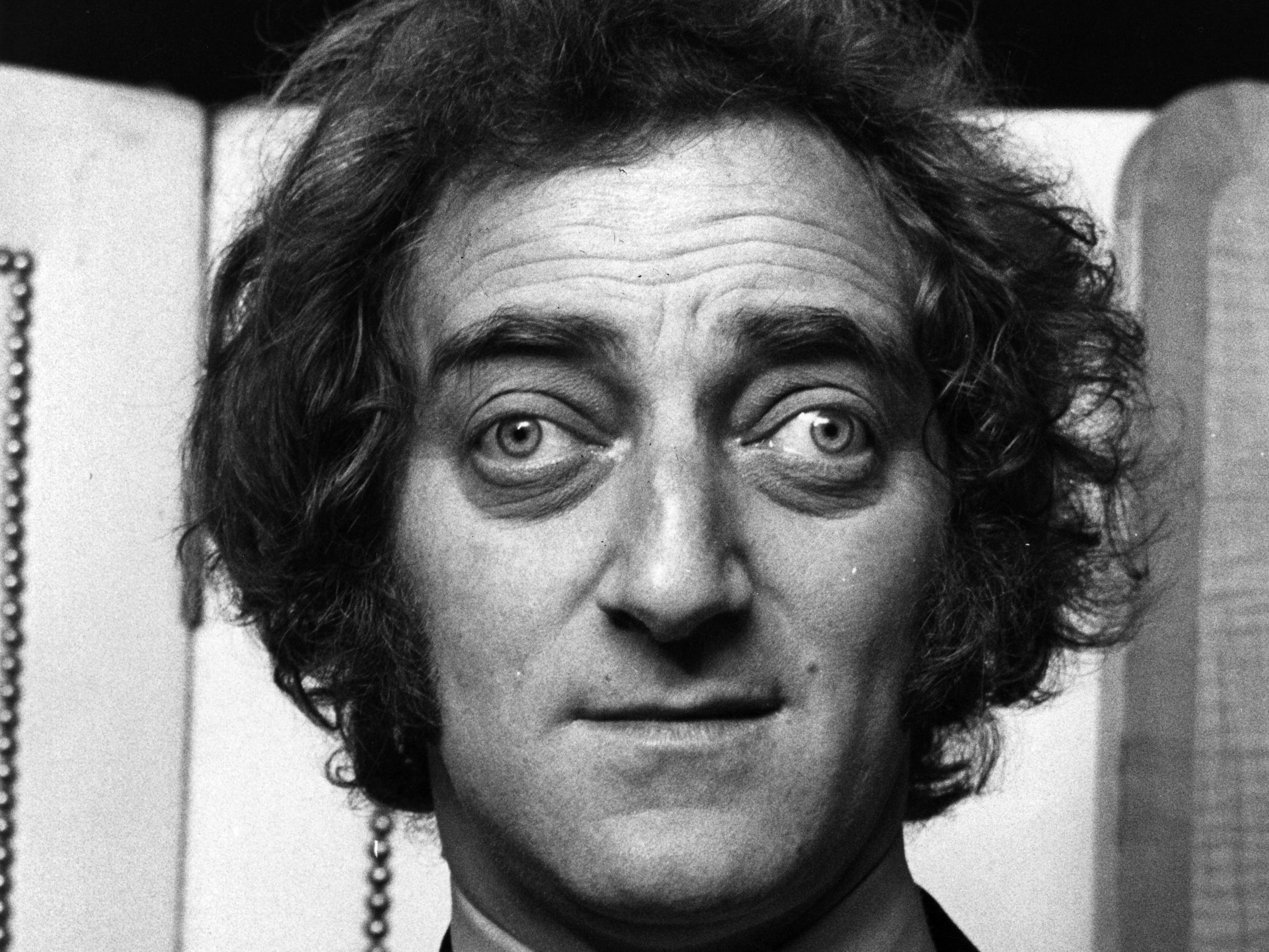
For our secondary analysis, we examined individual autoimmune disorders. We found the likelihood of having psychosis was higher for pernicious anaemia, pemphigoid (a disease characterised by skin blisters), psoriasis, coeliac disease and Graves’ disease (the disease suffered by Marty Feldman that causes protrusion of the eyeballs).
But it was lower for rheumatoid arthritis and ankylosing spondylitis (a type of arthritis that mainly affects the spine), suggesting that these disorders are protective.
There are a range of possible mechanisms that might underlie the relationships we found. Given that people with psychosis have also been found to show higher levels of inflammatory markers in the blood than healthy people, and that inflammation is a core feature of autoimmune disorders, inflammation is a likely candidate.
But rheumatoid arthritis and ankylosing spondylitis are also characterised by higher levels of inflammation, so this would not explain the negative relationships we found with these disorders.
Although all autoimmune disorders activate the body’s immune system, the exact response differs depending on the disorder. This might go some way to explaining why we found different relationships for individual autoimmune disorders, and suggests that inflammation cannot be the only mechanism.
It is possible that there might be a genetic link between autoimmune disorders and psychosis. In fact, research has recently shown that variations within specific genes are associated with both schizophrenia and rheumatoid arthritis.
That is, people with one variation of the gene are at risk for schizophrenia, while people with the other variation are at risk for rheumatoid arthritis. This might explain why rheumatoid arthritis appears to be protective for psychosis.
Newly discovered antibodies (part of the immune system’s armoury) that go rogue and mistakenly attack brain cells might also explain the link. These sorts of antibodies are thought to cause psychotic symptoms, such as paranoia and hallucinations, in some people.
Although our study cannot tell us why autoimmune disorders and psychosis occur together more commonly than we would expect, it provides stronger evidence that a relationship does exist.
Our group is involved in further research to help us better understand the mechanisms that might underlie this complex relationship.
So what is the real-world application of these findings? Although the risk of psychosis is only slightly increased for people with autoimmune disorders, our findings suggest that perhaps doctors ought to monitor people with certain autoimmune disorders for early signs of psychosis – especially pernicious anaemia, Graves’ disease and pemphigoid, which showed the most consistent relationships with psychosis.
This is important because early intervention has been shown to improve long term outcomes for people in the initial stages of a psychotic disorder.
is a Sir Henry Wellcome post-doctoral fellow and honorary lecturer at King’s College London. This article was originally published on TheConversation.com
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks