Teenage mental-health crisis: Rates of depression have soared in past 25 years
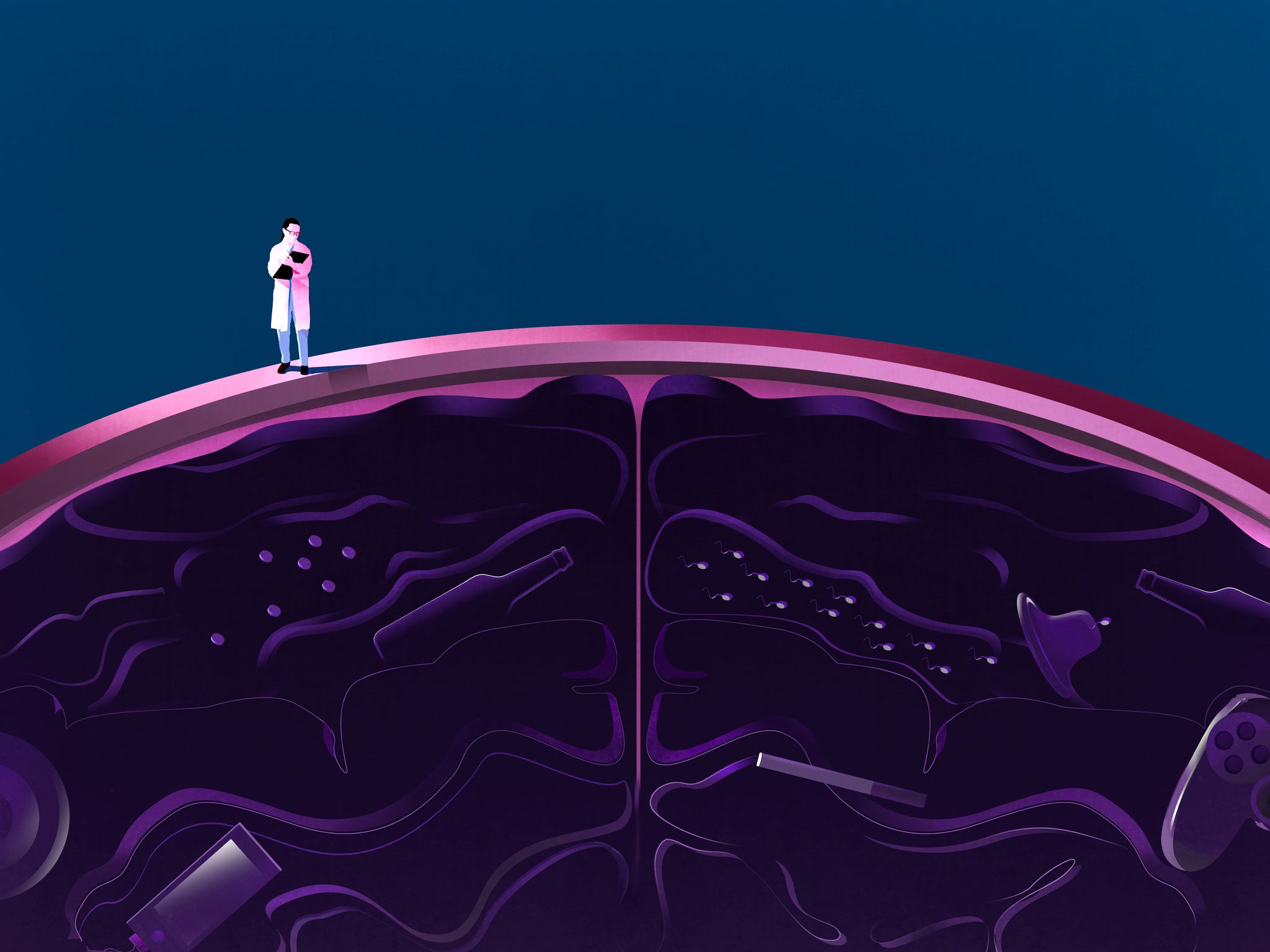
How has society managed to produce a generation of teenagers in which mental-health problems are so prevalent?
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.On most counts, young people's lives are improving. Drinking, smoking and drug-taking are down in the UK; teen pregnancies are at their lowest level for nearly half a century. Yet there is growing evidence that teens are in the grip of a mental-health crisis. It is as if, rather than acting out, young people are turning in on themselves.
Rates of depression and anxiety among teenagers have increased by 70 per cent in the past 25 years. The number of children and young people turning up in A&E with a psychiatric condition has more than doubled since 2009 and, in the past three years, hospital admissions for teenagers with eating disorders have also almost doubled. In a 2016 survey for Parent Zone, 93 per cent of teachers reported seeing increased rates of mental illness among children and teenagers and 90 per cent thought the issues were getting more severe, with 62 per cent dealing with a pupil's mental-health problem at least once a month and an additional 20 per cent doing so on a weekly or even daily basis.
For parents and teachers this is a difficult thing to confront: an epidemic of young people at odds with the world around them is hardly a positive reflection of the society we've created for them. When young people's mental health is discussed, there tends to be a lot of hand-wringing about the lack of early help and the long waiting times for clinical support – which is fair enough, because until the Government announced new funding last month, child and adolescent mental health services (CAMHS) received less than 0.6 per cent of the total NHS budget. But perhaps the more interesting question is why is there a crisis in the first place?
With celebrities (Stephen Fry, Ruby Wax, Alastair Campbell) increasingly talking openly about their own mental illnesses, there is much greater awareness than there used to be and correspondingly less stigma, making it easier for teenagers to acknowledge their problems. This undoubtedly skews the figures (insofar as there are figures: we were very bad at measuring young people's mental health in the past). But even if you accept that there's more reporting than there was a decade or two ago, pretty much everyone agrees that something very disturbing is happening.
Those who are worried include David Cameron, the first Prime Minister ever to have talked about teenage mental health. Last month he personally announced new money and the introduction of waiting times for teenagers with eating disorders. The Duchess of Cambridge has also made young people's mental health one of her major interests. A Girl Guides' attitudes survey found that mental health was one of the most pressing concerns, with 62 per cent of those surveyed knowing a girl their age who has struggled with mental-health problems.

Mental illness can feel like a personal indictment to parents. It is known that children who are looked after by their local authority are particularly susceptible and, conversely, that there are protective factors linked to a stable home life. Nonetheless, children are often reluctant to talk to their parents, and parents slow to respond, despite the fact that swift intervention is important to recovery. But there's no point in parents blaming themselves: mental illness is caused by a combination of factors and it can strike anywhere. Being middle class, affluent, in a two-parent household, loved, cherished, and successful at school is no guarantee of anything.
Fixers, the charity offering young people the opportunity to create media campaigns, says that 69 per cent of the 18,000 young people they have worked with have wanted to raise awareness of mental health. "We're a barometer of young public opinion," says CEO Margo Horsley, "and the resounding majority want to show people the tough realities of living with anxiety, depression, self-harm, anorexia, bulimia, diabulimia, body dysmorphia, binge-eating disorder … the list goes on." The stories of many of the young people they have worked with suggest that when mental illness strikes, it feels elemental, chemical and incomprehensible; they commonly liken it to possession.
That doesn't mean that we shouldn't query whether there are things going on to do with the way we live our lives. Unhappiness and depression are concentrated in highly unequal societies. In his book The Happiness Industry, William Davies assembles evidence (including from Wilkinson and Pickett in The Spirit Level and Carles Muntaner of the World Health Organisation) to demonstrate that strongly materialist and competitive values lead to higher levels of mental distress. When people feel buffeted by forces over which they have no control, he argues, we conclude it is they who need correcting, rather than the forces: "In the long history of scientifically analysing the relationship between subjective feelings and external circumstances, there is always a tendency to see the former as more changeable than the latter."

Research by the mental-health charity Young Minds has found that exams are a significant trigger for mental illness in young people. Under pressure to get the best possible results, schools are inclined to give teenagers the impression that they have only one shot at tests that will determine the rest of their lives (even though this is not true). The anxiety transmits itself to parents – and this, according to Julie Lythcott-Haims, former dean of freshmen at Stanford and the author of How to Raise an Adult, is having a direct impact on young people's mental health, as parents strive to maximise their children's accomplishments, seeing them as an indication of their own value.
Responsibility for your parents' sense of self-worth is a heavy burden to bear. Natasha Devon, the Government's first ever mental-health champion for schools, who runs workshops through her organisation Self-Esteem Team, says she often encounters young people at independent schools who are "hyper-aware of how much parents have spent on their education and of the expectation that they will go on to university".
The American College Health Association surveyed 100,000 college students at 53 US campuses and found that 84 per cent of US students feel unable to cope, 79 per cent are exhausted, 60 per cent feel very sad and more than half are experiencing overwhelming anxiety. Lythcott-Haims directly links these staggering conclusions to the way that children have become a project, not just in themselves, but also for their parents' egos.
American (or indeed British) students may well be wondering what all their effort is for exactly. Yale professor Bill Deresiewicz has characterised the current generation of high-achieving students as "excellent sheep", haunted by a fear of failure yet clueless about where they're going. They're probably worried that it's nowhere: the OECD's projections for the world economy between now and 2060 are for slowing world growth and near-stagnation in advanced economies. The Oxford Martin School has predicted that 47 per cent of US jobs are susceptible to automation. Sarah Brennan, chief executive of Young Minds, says her organisation is seeing children as young as 11 worrying about unemployment.

We are educating young people for a world that is unlikely to exist in 20 years' time and, arguably, not equipping them with the skills they need for the one that will. And then there's the internet, which has grown up at the same time as the explosion in teen mental illness, and is often seen as part of the problem, with cyberbullying and worries about body image (created partly by selfie culture) often cited as triggers.
Social media doesn't create bullying or anxieties about body image (it's worth noting that rates of bullying haven't risen in the last 10 years). But technology can amplify problems or give them new forms of expression. Cyberbullying can be particularly painful. But the trouble with seeing social media as the problem is that it's the technology that then gets addressed rather than the underlying issues. And after the digital detox, the problems remain.
For most people, the effects of technology are noticeable in the changes, mostly small but cumulative, in our moods, manners, feelings and ways of going about our lives. Facebook's famous experiment, published in July 2014, in which it doctored the feeds of some of its users to spread unhappiness, proved that social media can affect our moods (as if we needed proof that Facebook makes us feel as though everyone else is eating better food and hanging out with cooler people than we are). The curated lives displayed online can make anyone feeling even slightly vulnerable feel really wretched.
That said, social media can also provide support for young people, especially for those struggling with their sexuality (44 per cent of 16-24 year-old LGBT people have considered suicide) or feeling isolated. Technology is an easy target for adults: it's new, it moves faster than we do and it's very visible in young people's lives. But it may be that some of the energy adults spend worrying about technology would be better spent worrying about the world that creates and shapes both social media and the psyches of our children.

There is much about mental illness that may well be very difficult to prevent: biological susceptibility, unavoidable triggers like bereavement. It makes sense to focus on the dearth of early-stage therapies that are known to make a difference because, at the moment, as Brennan says, "we are investing in having a sick adult population: 75 per cent of adult mental illness emerges before the age of 25 and only 50 per cent of young people are getting any kind of care."
Still, when you are tackling an epidemic, you need to think about more than treatment. We also need to ask hard questions about why children feel so at odds with a world that ought, after all, to be all about them and their future.
CASE STUDY 1:
Jordan Caldwell, 18
Carnmoney, Co Antrim
I was diagnosed with anorexia at the age of 12. My grandad and two uncles had died in a short space of time. I was representing Northern Ireland in football matches; I got a call saying they didn't want me back. I decided it was because I was too fat. I'd always been a big strong lad for my age but I thought if I lost a bit of weight I'd be able to play at the top level again.
For a while my mum and dad thought I was just being faddy. I wish I had been able to talk to someone before the thoughts became so strong but I didn't want to. Then one day my mum saw me coming out of the shower and she was horrified. My parents took me to the GP, who referred me to the eating disorders clinic. On my first visit they did some tests, bloods and blood pressure and so on, and said I was too ill to go home. I had two months in hospital. They didn't know what to do. I still wasn't eating.
After I was discharged, I was very abusive. I was constantly shaking and screaming. I would try and hit my head on things. I'll never forgive myself for what I put the family through. My little sister was afraid to say hello to me. The anorexia was like demons inside my head, telling me what to do. My mum says I vanished. She said she saw me fighting every day and if it had been a person I was fighting, she would have killed them.
I hadn't eaten or drunk anything or brushed my teeth for a week – I thought the toothpaste had calories in it – when I had a seizure. It was my 14th birthday. The doctors said afterwards it was a miracle I survived. I went into a psychiatric hospital for 11 and a half months. My little sister had to go and live with my granny because my parents were with me 10 hours a day and the hospital didn't want her to see me in the state I was in.
Eventually I started to make signs of improvement – I could talk the talk – but when I was discharged the nurses predicted I'd be back in a couple of weeks. I was up and down after that but I was determined to stay out of the hospital. I wanted my sister to be able to stay at home. The illness tried to tear the family apart. It came very close.
I went three or four times a week as an outpatient to the CAMHS eating disorders clinic. I got a personal trainer, who helped me to exercise and talked about the need to put food into your body to do that. When he first came to see me there was a mark in the carpet where I'd been doing sit-ups so frantically. I needed someone to be harsh with me. Up until then, if I argued with Mum and Dad, I wouldn't eat. Now I am working at the gym as a receptionist and I've just passed my level 2 to be a gym instructor. I still ask "why me?" and I don't know the answer. I feel it's important to talk about it, though. If I can help one other person, that would be something.
CASE STUDY 2:
Cerys Pumphrey, 18
Bournemouth
The crisis came when a pen that had been in someone's mouth a week or two earlier touched my cheek. I burst into tears. I was in absolute panic; I felt I was going to be sick. My heart was in my throat: it was like when you hear that a close family member has died. I was about 16 and the stress of GCSEs was really kicking off.
I can't pinpoint the first symptoms of my OCD: it's a voice in my head, like the voice of conscience, and when I was younger I had the power to shut it out. By the time I was 16 I couldn't control it. I think there is a biological aspect to it: I have OCD, my cousin has depression, and they are both linked to low levels of serotonin. But there has to be a trigger and for me it was the stress of exams.
After the pen incident I talked to my mum but it was very difficult for her to understand: I was playing rugby, I'd done my Duke of Edinburgh; in her mind there was no way I could have a mental-health issue. I booked an appointment with the GP and I'd been there about two minutes before they said I needed to be referred to Child and Mental Health Services (CAMHS). I think it was because of my hands: it was December and every winter they get cracked and dry to the point that I can't move them, because I am washing them so many times a day – about 30 times, usually.
I was really lucky: I only had to wait about two months for my CAMHS appointment. The whole thing was a massive shock to my family: they didn't know how to take it. The first year with CAMHS I was a mess. I kept having panic attacks. They'd come on if someone brushed past me who I thought was dirty, or if I thought I was sitting down on a bodily fluid. Most people call their voice something like "devil", but I called mine Helen.
When I turned 18, I was discharged from CAMHS. They really helped me sort out some of my weaker compulsions but we weren't able to get to the handwashing. I'm with the adult service now. At my last therapy session my psychologist said that CBT (cognitive behavioural therapy) could well work for me.
I told people once I started going to CAMHS. I wasn't going to keep it secret. A lot of people thought I was attention-seeking and some people didn't believe me. It annoys me when people say, "I'm a little bit OCD," because it's not a joke. I struggle to explain why I do certain things. I have to wash my hands up to my forearms in school. It looks very weird, washing half my arm. I use a lot of soap and I have to wash three or four times before I can leave the toilet. Sometimes I have to wash my bag if it touches something I think is dirty. It's very lonely.
I am doing A-levels now and I've applied to do history at university. The universities I've applied to have very good mental-health services; that was one of my main criteria. It will be hard to adjust, but I think I will be safe.
CASE STUDY 3:
Naomi Lea, 17
St Asaph, Denbighshire
I realised there was something wrong when I was 14. I was increasingly stressed about exams and I was having panic attacks in school and couldn't stay in lessons. I was predicted all As and A*s at GCSE but my self-esteem was so low, I didn't think it was possible. I became terrified that teachers would ask me a question in class.
I started self-harming. I hid it very well; no one was aware of what I was doing. I went very quiet and I wouldn't socialise or speak in class. My teachers thought it was because I was shy.
In Year 11, just before my GCSEs, I decided I'd had enough and I spoke to a teacher about how I was feeling. Once I had opened up, the school got me a referral to CAMHS. I had to wait about six months for an appointment – there was a horrendous waiting list – and I had four sessions with a counsellor in school in the mean time.
I really struggled with the first few exams. I would lose concentration and go blank. As they went on I would get really really anxious beforehand but, once I was there, I could manage. Eventually, about a year ago, when I started with CAMHS, we did tell my mum. She was really understanding. She's a single parent – or she was then, she's in a relationship now. It's very difficult for parents to deal with.
Once I got through the waiting list, I had quite a good relationship with my psychologist and I had a course of CBT which was really helpful: I learnt skills that helped me manage my anxiety. When they discharged me, I felt I wasn't ready but they wanted me to see if I could deal with it alone. For the first few months I felt I was managing, but things have gone downhill again recently, possibly because I'm coming up to A-levels. I'm on the horrible waiting list again.
I've applied for university and I'm hoping that independence will help me to learn to control it better. The whole time I was in school, I never had a lesson about mental health. I saw a post online about a project with [mental-health support group] Fixers and I wanted to make a film that could be shown to students in the early years of secondary school, about recognising the signs. I have run a workshop with it at school and shared it on Facebook and it was shown on ITV news.
The online world was my support network. Most of the time, it was really helpful. I made friends I could talk to regularly and it gave me someone to rant about my day to at a time when I couldn't tell my school friends. I thought they would judge me.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments