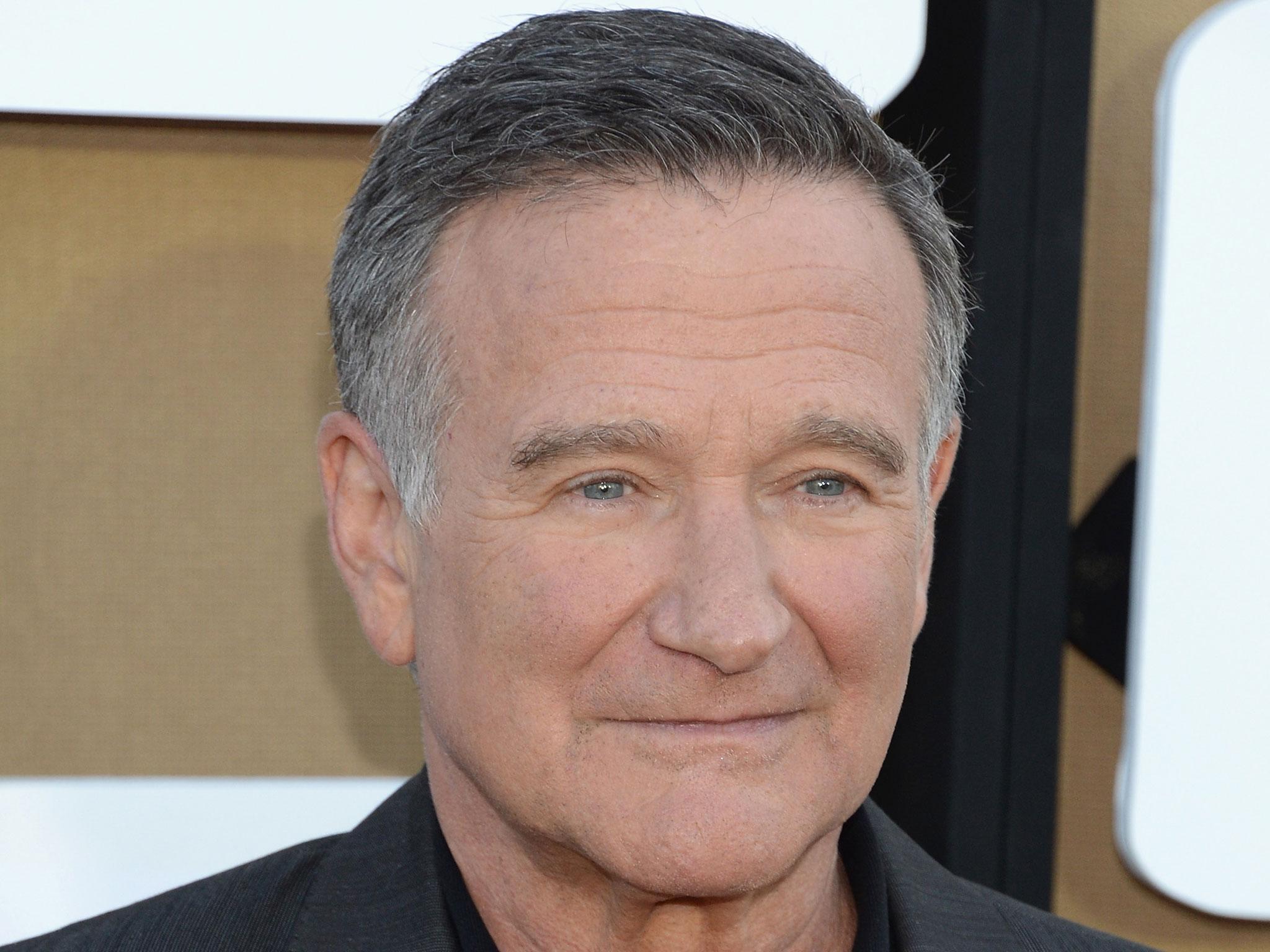
What is Lewy Bodies Dementia, the condition Robin Williams was diagnosed with after his death?
Coroners discovered signs of Lewy Bodies Dementia in Robin Williams' brain
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Depression, paranoia, Parkinson’s disease, confusion and dementia. The long list of symptoms suffered by Robin Williams is itself confusing, but all of these and more besides, can be accounted for by the disorder bearing the name, dementia with Lewy bodies (DLB), which his widow has now announced as his final diagnosis.
Few people have heard of DLB until, like Williams' family, they are confronted by its multiple and variable combinations of symptoms which fluctuate in severity in an alarmingly unpredictable manner.
Yet DLB is the second most common cause of dementia in older people, accounting for 10-15% of all dementia cases and affecting at least 100,000 people in the UK alone. Only Alzheimer’s disease itself is more common.
Despite this, as the founder of the Consortium on Dementia with Lewy Bodies which has, over two decades, developed global consensus on guidelines for the clinical and pathological diagnosis and management of this common disorder, I am aware how little-known it is.
A strange and shocking illness
Lewy bodies were first described in the early 20th century by Dr Friedrich Lewy, who was studying the brains of people with Parkinson’s disease, a condition recognised by a combination of a shaking tremor, slowness of limb movements, and a shuffling walk.
Lewy bodies are, in fact, microscopic clumps of a protein called alpha-synuclein which may, under certain and as yet not understood circumstances, accumulate within nerve cells in the brain. When some critical brainstem and midbrain structures including the substantia nigra are involved, there is a loss of the neurotransmitter dopamine and Parkinson’s disease is the result.
But in the last 20 years or so, we have realised that Lewy body disease can also affect other parts of the brain, producing symptoms other than those of Parkinson’s. It occurs in the autonomic and peripheral nervous system producing vegetative symptoms such as low blood pressure, constipation and sweating.
Defining symptoms
Lewy bodies occurring in the cerebral cortex, meanwhile, lead to the characteristic symptoms by which DLB is recognised, usually starting with mild and fluctuating disturbances in attention and wakefulness.
The affected person appears vague, drowsy or frankly confused with a decrease in their interest and ability to reason or to carry out practical tasks. Apathy is one term used for this and is frequently mistaken for depression.
Visuo-perceptual function is also affected early which may account for the report of Williams’ bruising “miscalculation with a door”, and it is this involvement of the visual system which underpins the occurrence of the lifelike visual hallucinations which occur in about 80% of cases and often alert the clinician to a DLB diagnosis.
Waking nightmares
Hallucinations may be threatening or distressing but are often simply perplexing for patients who cannot understand why familiar faces or unknown intruders repeatedly appear to them. For others, the hallucinations occur as nightmares as part of a specific sleep disorder. As the Lewy body pathology disease progresses, generalised cognitive impairment and dementia progressively worsen, although a fluctuating pattern with intervals of lucidity often persists.
Parkinsonism occurs in many but by no means all sufferers and in those like Robin Williams in whom it seems to have been quite early and prominent, the initial diagnosis given is often one of Parkinson’s disease, a dementia label following soon after as additional symptoms emerge. Short-term memory failure, the hallmark of Alzheimer’s disease may not be prominent unless, and here’s where it starts to get complicated, there is also a lot of Alzheimer’s disease pathology in the brain as well.
Hard to pin down
Why did it take so long to recognise the existence of DLB, especially if it is so common? The answer, is that cortical Lewy bodies are vanishingly difficult to see in the brain using conventional staining methods, unlike their brainstem counterparts observed so long ago by Dr Lewy.
Nevertheless, the development of immuocytochemical staining methods in the early 1990s suddenly made them visible outside of specialised units. This was a major step forward.
But what progress is the research community making with DLB now? Internationally agreed criteria for the clinical and pathological diagnosis have been agreed since a meeting held in Newcastle upon Tyne in 1995, updated there in 2005 and due to be reviewed and updated again in December this year.
Dedicated research centres such as the NIHR-funded Biomedical Research Unit in Lewy Body Dementia at Newcastle University have led the field by, for example, developing diagnostic tests such as the dopamine transporter SPECT scan, which can distinguish DLB from Alzheimer’s with >85% accuracy and which is now widely clinically available.
New hope
Therapeutic trials have been few and far between in DLB because of a combination of a lack of compounds to test, a pre-occupation with targeting Alzheimer’s and a reluctance of regulatory bodies to recognise DLB. All of these are now changing and DLB is increasingly viewed as a malleable and commercially-viable target.
Pharmacological trials in DLB will undoubtedly increase public awareness and for families such as Robin Williams’ there are now highly-effective patient and carer organisations that provide information, advice, advocacy and support research activity.
As an inter-form of Parkinson’s and Alzheimer’s disease, DLB has the potential to unlock the key to both of its related disorders. It is high time it was put in the spotlight.
Ian McKeith, Professor of Old Age Psychiatry, Newcastle University
This article was originally published on The Conversation. Read the original article.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments