The pacemaker for the brain that could finally cure depression
’If I hadn’t had DBS, I’m pretty sure I would not be alive today’
Emily Hollenbeck lived with a recurring depression she likened to a black hole, where gravity felt so strong and her limbs so heavy she could barely move. She knew the illness could kill her. Both her parents had taken their lives.
She was willing to try something extreme: Having electrodes implanted in her brain as part of an experimental therapy.
Researchers say the treatment — deep brain stimulation, or DBS — could eventually help millions with depression that resists other treatments. It's approved for conditions including Parkinson's disease and epilepsy, and many doctors and patients hope it will become more widely available for depression soon.
The treatment gives patients targeted electrical impulses, much like a pacemaker for the brain. A growing body of research is promising, with more underway — although two large studies that showed no advantage to using DBS for depression temporarily halted progress, and some scientists continue to raise concerns.
Meanwhile, the Food and Drug Administration has agreed to speed up its review of Abbott Laboratories' request to use its DBS devices for treatment-resistant depression.
“At first I was blown away because the concept of it seems so intense. Like, it’s brain surgery. You have wires embedded in your brain,” Hollenbeck said. “But I also felt like at that point I tried everything, and I was desperate for an answer.”

Hollenbeck suffered from depression symptoms as a child growing up in poverty and occasional homelessness. Her first major bout happened in college, after her father’s suicide in 2009. Another hit during a Teach for America stint, leaving her almost immobilized and worried she’d lose her classroom job. She landed in the hospital.
She calls it “an on-and-off pattern.” After responding to medication for a while, she'd relapse.
She earned a doctorate in psychology, even after losing her mom in her last year of grad school. But the black hole always returned. At times, she said, she thought about ending her life.
She said she'd exhausted all options, including electroconvulsive therapy, when a doctor told her about DBS three years ago.
“Nothing else was working,” she said.
She became one of only a few hundred treated with DBS for depression.

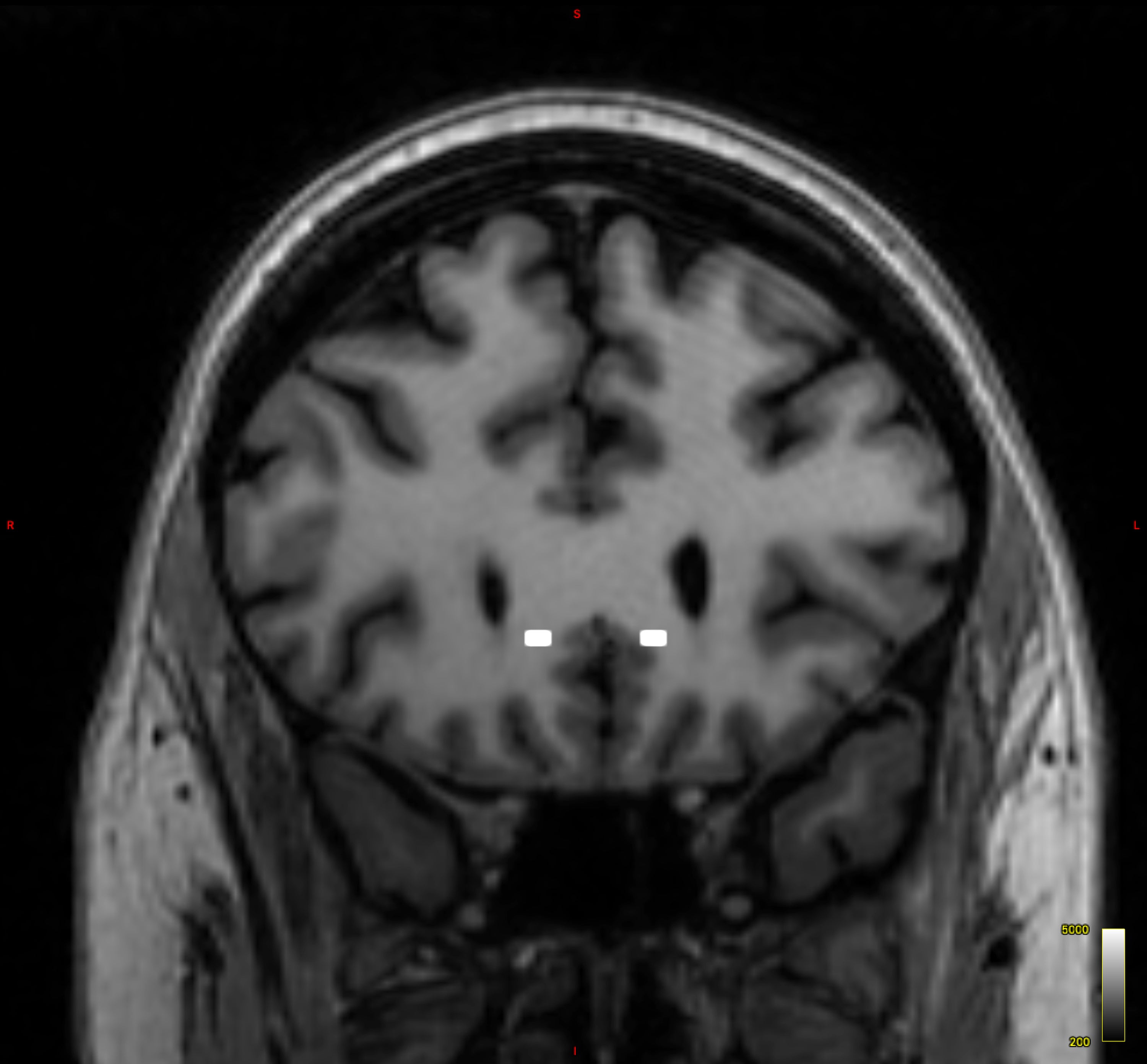
Hollenbeck had surgery while sedated but awake. Dr. Brian Kopell, who directs Mount Sinai's Center for Neuromodulation, placed thin metal electrodes her brain's subcallosal cingulate cortex, which regulates emotional behavior and is involved in feelings of sadness.
The electrodes are connected by an internal wire to a device placed under the skin in her chest, which controls the amount of electrical stimulation and delivers constant low-voltage pulses.
Doctors say electricity speaks the brain’s language. Neurons communicate using electrical and chemical signals.
In normal brains, Kopell said, electrical activity reverberates unimpeded in all areas, in a sort of dance. In depression, the dancers get stuck within the brain’s emotional circuitry. DBS seems to “unstick the circuit,” he said.
Hollenbeck said the effect was almost immediate. She only wishes the therapy had been there for her parents.

The road to this treatment stretches back two decades, when neurologist Dr. Helen Mayberg led promising early research.
But setbacks followed. Large studies launched more than a dozen years ago showed no significant difference in response rates for treated and untreated groups.
Some later research, though, showed depression patients had stable, long-term relief from DBS when observed over years. Overall, across different brain targets, DBS for depression is associated with average response rates of 60%, one 2022 study said.
Mount Sinai's team is one of the most prominent researching DBS for depression in the U.S. There, a neuroimaging expert uses brain images to locate the exact spot to place electrodes.
“We have a template, a blueprint of exactly where we’re going to go,” said Mayberg, a pioneer in DBS research and founding director of The Nash Family Center for Advanced Circuit Therapeutics at Mount Sinai.
Other research teams also tailor treatment, although methods differ slightly.
Abbott is launching a big clinical trial this year, ahead of a potential FDA decision.
But some doctors are skeptical, pointing to potential complications such as bleeding, stroke or infection after surgery.
Dr. Stanley Caroff, a University of Pennsylvania emeritus professor of psychiatry, said scientists still don't know the exact brain pathways or mechanisms that produce depression. And it's also tough to select the right patients for DBS, he said.
“I believe from a psychiatric point of view, the science is not there,” he said of DBS for depression.
Hollenbeck acknowledges DBS hasn't been a cure-all; she still takes medicines for depression and needs ongoing care.
She recently visited Mayberg in her office and discussed recovery. “It’s not about being happy all the time,” the doctor told her. “It’s about making progress.”
That’s what researchers are studying now — how to track progress.
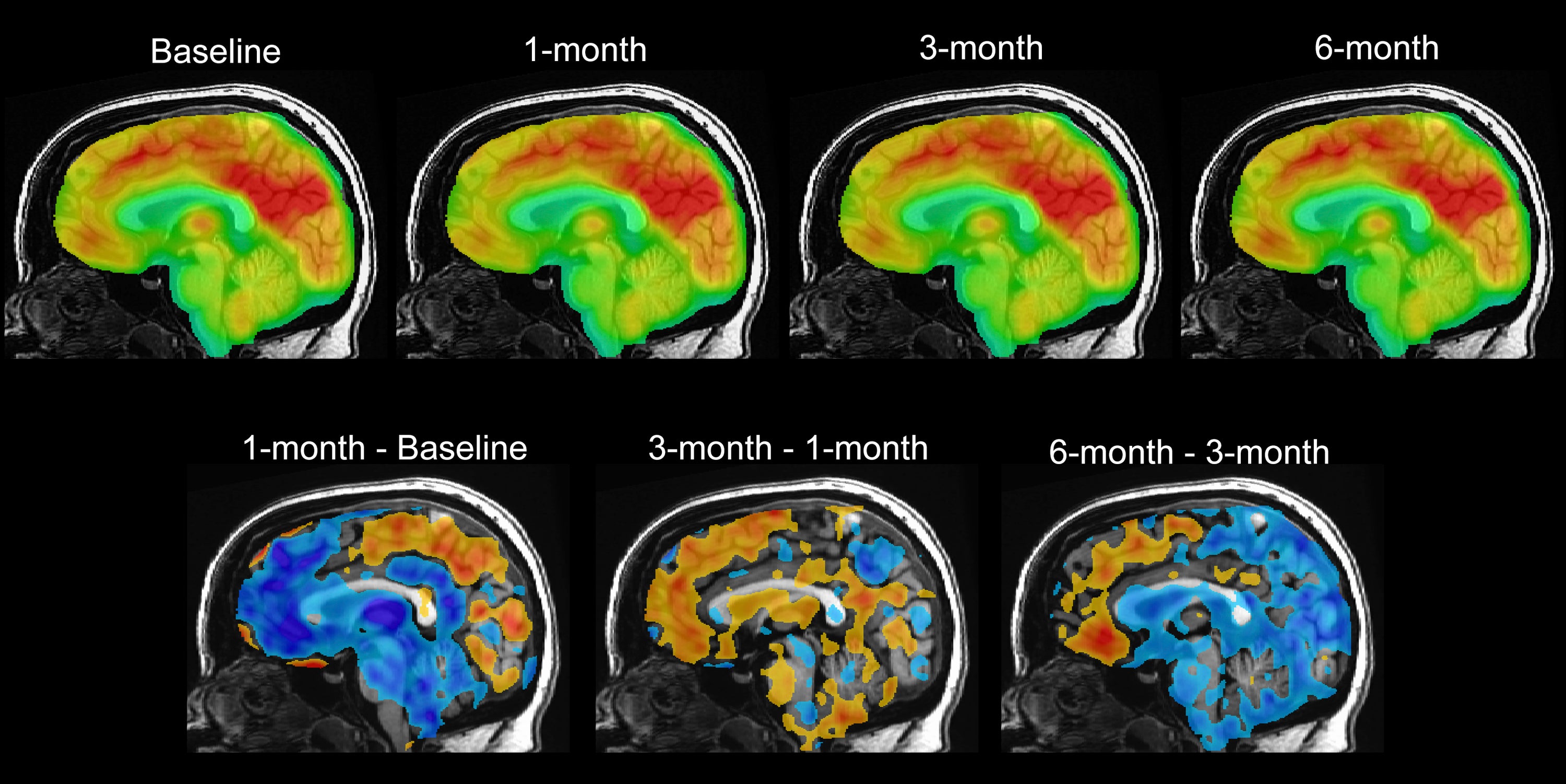
Recent research by Mayberg and others in the journal Nature showed it’s possible to provide a “readout” of how someone is doing at any given time. Analyzing the brain activity of DBS patients, researchers found a unique pattern that reflects the recovery process. This provides an objective way to observe people's improvement and distinguish between impending depression and typical mood fluctuations.
Scientists are confirming those findings using newer DBS devices in a group of patients that includes Hollenbeck.
She and other participants do their part largely at home. She gives regular brain recordings by logging onto a tablet and putting a remote above the pacemaker-like device in her chest. She answers questions about how she feels. And she records videos, analyzed for such things as facial expression and speech.

Occasionally, she goes into Mount Sinai’s “Q-Lab,” where scientists do quantitative research collecting all sorts of data, including how she moves in a virtual forest or makes circles with her arms. Like many other patients, she moves faster now that she’s doing better.
On a recent morning, Hollenback brushed her hair aside to reveal scars on her chest and head from DBS surgery — signs of how far she’s come.
She takes walks in the park and visits libraries, which were a refuge in childhood. She no longer worries that normal life challenges will trigger crushing depression.
“If I hadn’t had DBS, I’m pretty sure I would not be alive today," she said.
Bookmark popover
Removed from bookmarks