Scientists say routine test could detect those with high risk of blood cancer
Blood cancer is the fifth most common cancer in the UK
Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.A routine blood test may be able to detect patients who are at high risk of developing blood cancer, new research has found.
Blood cancer is the fifth most common cancer in the UK with around 41,000 people diagnosed with the disease each year.
The most common groups of blood cancer include leukaemia, lymphoma and myeloma.
The study, by scientists at Institut Gustave Roussy in France and presented at the 34th EORTC-NCI-AACR Symposium on Molecular Targets and Cancer Therapeutics in Barcelona, Spain, took blood samples from 1,416 patients with various solid tumours and found that eight per cent of those tested were at higher risk of blood cancer.
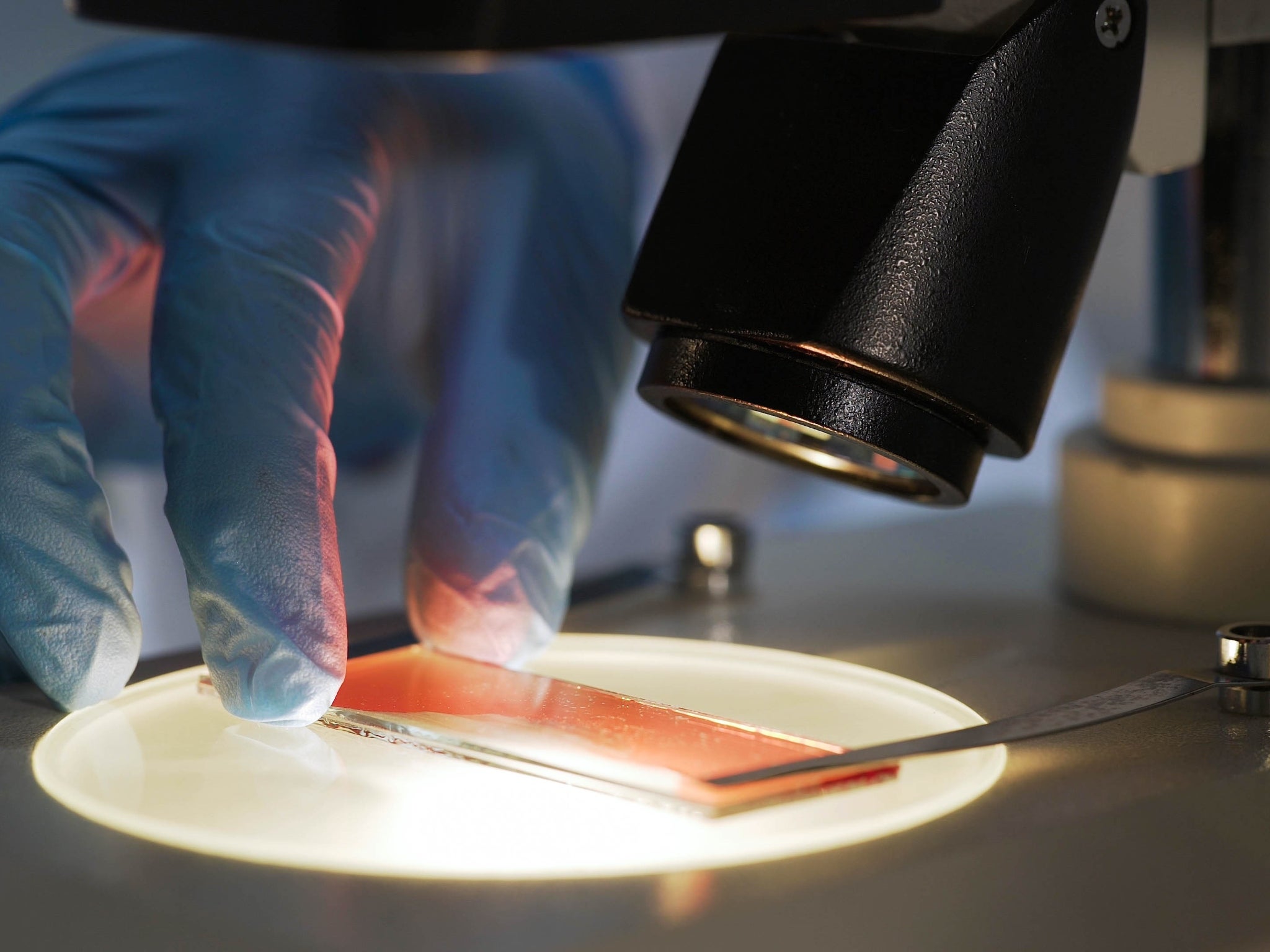
At present, blood samples are currently used to identify cell-free DNA (cfDNA) which is caused by tumours shedding DNS into the blood.
These samples can allow doctors to better characterise the cancer, select the best therapy, and monitor how the disease is progressing.
A condition called clonal haematopoiesis (CH) is commonly found in blood samples and paved the way for even more diagnostic possibilities.
Normally, haematopoietic stem cells create other blood cells from the bone marrow.
However, CH occurs when a haematopoietic stem cell starts creating stem cells with a different genetic pattern to normal blood cells.
The cells can then shed DNA into the blood and previous research shows there is a one percent chance CH will progress to blood cancer each year.
As a result the scientists wondered if the blood samples could be used to identify patients who have developed blood cancer or are likely to do so.
They tested the tests for myelodysplastic syndrome and acute myeloid leukaemia.
Myelodysplastic syndrome is a blood disorder originating in bone marrow, and it can develop into white blood cell cancer acute myeloid leukaemia.
The researchers believed when a blood sample revealed high-risk CH doctors should study the blood to identify the likelihood it will become blood cancer, or whether it has already turned to blood cancer.
“We found that 113 patients, or eight per cent, had at least one clonal haematopoiesis mutation that could be considered to place them at higher risk of developing blood cancers during their life,” one of the researchers, Dr Marco Tagliamento, said.
“Out of these patients, 45 were referred to our haematology unit by their oncologist and five were subsequently diagnosed with blood cancer: one with myelomonocytic leukaemia, two with myelodysplastic syndrome and two with essential thrombocythaemia.”
Tagliamento added that this early detection of blood cancer could prevent complications during anti-cancer treatments and it could also “indicate possible diagnostic and therapeutic pathways for doctors to consider for haematological disease”.
Tagliamento continued: “Case-by-case evaluation is crucial. Different aspects must be considered when evaluating the potential impact and management of high-risk clonal haematopoiesis in patients who already have cancer.
“These relate, for example, to the patients, their medical history and to the underlying cancers. All of them should be part of a balanced evaluation made for each individual case.”
Professor Ruth Plummer, of Newcastle University, said: “This is well-conducted research that reveals an additional facet to the information gained from liquid biopsies.
“Dr Tagliamento is right to stress the importance of evaluating the context for each individual patient. Cancer patients have much to worry about, and so their doctors need to take into account the patient’s clinical situation and their treatment plan.
“Patients’ anxieties mean that it will not always be appropriate to highlight a potential increased risk of developing an additional blood cancer in later years. Only some specific clonal haematopoiesis mutations are likely to predict a higher risk of blood cancer developing at some point in the future."
She added: “This study suggests patients with these mutations should be referred for further evaluation and even then, decisions about what would be best for these patients will depend on a range of other factors.”
Additional reporting by SWNS







Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments