Britain’s past holds the key to breaking the deadly cycle of heroin addiction and crime
The UK was once a world leader in treating drug addiction. As our own crisis spiralled out of control, other countries looked to our past for a solution. Their success is forcing Britain to rethink its approach in the war against drugs, writes Andy Gregory


Heroin addiction casts a deadly shadow over Britain. Fatalities involving the drug have doubled since 2011, and now stand at their highest level since records began. Behind the statistics lie stories of people dying in their homes, hospitals and in the streets, leaving children, siblings and friends behind. Vulnerable users continue to be jailed for possession, or for committing crime to fund their use, while increasingly powerful and violent organised crime groups exploit children to pump the drug into every part of the country.
Britain’s “war on drugs”, which began nearly half a century ago, is failing. As drug users have entered prisons rather than treatment programmes, the cycle of addiction and crime has not just continued but taken an even tighter hold, with a boom in organised crime gangs now running supply lines from the cities into rural areas. So what is the answer to breaking the cycle? Where can we look for an alternative way to approach the issue?
The answer could lie in Britain’s own past. In 1926, heeding the advice of medical experts, the Conservative Party began prescribing heroin, paid for by the taxpayer, to great success – with countries across the world following suit. Indeed, the policy continues today on a far smaller scale. Hundreds of people across the UK are currently prescribed medical-grade heroin (diamorphine), quelling their need for unpredictable and sometimes deadly street drugs and taking power away from increasingly violent organised crime groups.
The Independent can reveal that 280 people received a diamorphine prescription in 2017-18, via a freedom of information request to Public Health England by Release, a charity offering drug-related legal advice and support. While more intensive than methadone, the drug is more successful at keeping people in treatment and away from street drugs, and can be a lifesaving tool for a small percentage of entrenched heroin users.
Dr Prun Bijral had about 70 patients as a frontline doctor in 2010, many of whom received prescription diamorphine. He is now medical director at the UK’s largest drug treatment provider, Change Grow Live. “I witnessed how it can help transform people’s lives and give them stability where previous things hadn’t been successful,” he says.
Although this figure now pales in comparison to the number of people receiving methadone (around 0.002 of patients are prescribed the drug), Britain successfully used heroin as its major form of treatment for 50 years. As it was the only country in the world to do so, this became known colloquially as the “British System”.
While a few hundred people have benefited from this legacy ever since, the memory of Britain’s pioneering approach has been largely forgotten – although the history remains as relevant as ever. Choosing to treat drug addiction as a health issue rather than a criminal offence, the government decided in 1926 to allow doctors with a Home Office licence to prescribe addicts with heroin and cocaine.
The British System continued successfully for decades. In America and mainland Europe, where prohibition was enforced and drug use considered a moral failure, heroin users were numbered in the hundreds of thousands. But in Britain, where medical-grade heroin was prescribed without judgment and obtained in chemists such as Boots, the number of known users rarely rose above 1,000 until the late 1960s. Organised crime groups are rumoured to have cast an eye at the potential UK market and declared it a non-starter thanks to the British System: why set up shop if the vast majority of demand is catered for free of charge by the government?
For decades Britain stood out as a bastion of sense against the moralising hysteria of the US, which worked hard to push most of the globe towards prohibition. Doctors urged the government to hold its nerve, but after years of lobbying from America, the UK finally succumbed.
In America, where prohibition was enforced and drug use considered a moral failure, heroin users were numbered in the hundreds of thousands. But in Britain, where medical-grade heroin was prescribed without judgment and obtained in Boots, the numbers rarely rose above 1,000
Coupled with this trans-Atlantic pressure was the revelation that a handful of doctors were hugely overprescribing heroin and fuelling a “grey market” (legally obtained drugs sold illegally), which led the Home Office to clamp down on the British System. One of the key culprits was Lady Isabella Frankau, a supposedly well-meaning but naive psychiatrist who reportedly doled out 600,000 heroin tablets in 1962 alone, attracting superstar clients including jazz star Chet Baker and singer Marianne Faithfull as her infamy grew.
Despite warnings from experts that it would simply open up the heroin market to exploitation by crime groups, the Dangerous Drugs Act was passed in 1967, which stopped GPs from prescribing diamorphine, leaving methadone and morphine as the only alternatives. The Act also legally entitled GPs to refer addicted patients to the Home Office, after which they could be offered diamorphine by specialist doctors in new “drug treatment centres”. But there were delays in the building of these specialist treatment centres, and those that eventually opened operated a policy to reduce the number of patients eligible for diamorphine.
The Home Office’s drugs chief at the time was Bing Spear, a figure so sympathetic and attuned to the needs of those he served that he was often spotted mingling in the queue for diamorphine at Boots in Piccadilly Circus, and apocryphally at one stage knew the name of every person in the UK on a heroin script. He would later lament that the government had simply clamped down on rogue doctors, rather than the system itself, and called the move “an unmitigated disaster”.

As the ready supply of legal heroin from GPs dried up, a vacuum appeared for organised crime to exploit. By the time the Misuse of Drugs Act 1971 came into effect two years later, solidifying Britain’s new commitment to prohibition and leading to tens of thousands being jailed merely for possessing the means to feed their addiction, the amount of black market heroin consumed in the UK outstripped that supplied legally in drug treatment centres.
Our “war on drugs” had begun. The heroin epidemic that unfolded over the following two decades is notorious. By the mid-1990s, nearly half a million people in the UK were addicted. Neil Woods, a former police detective who spent 14 years undercover infiltrating increasingly violent and widespread gang networks, has co-written a book detailing the British System called Drug Wars. He says most people in the grips of heroin dependence have three main ways of funding a habit: they can allow themselves to be sexually exploited, they can steal or, vitally, they can find new customers.
Woods believes the heroin epidemic was largely caused by the demise of the British System. Organised crime stepped in with a tactic of encouraging users to become dealers and fund their own use by turning new people on to the drug, at a time when war in Afghanistan stimulated unprecedented supply to Margaret Thatcher’s Britain.
Heroin prescriptions were anathema to this tactic, as proven by one doctor who laboured to hold back the tide. From 1988 to 1998, Dr John Marks prescribed smokeable diamorphine to around 450 people in Merseyside. Rather than fuelling use, Dr Marks reported that Widnes, where his clinic was based, had 12 times less heroin addicts than neighbouring Bootle, while burglary and theft quickly dropped by 93 per cent. As the epidemic claimed lives across the country, Dr Marks’ clinic saw no drug-related deaths.
But as the clinic drew international media attention, central and local government were spooked. Dr Marks was blacklisted and his clinic shut down. At least 41 of his patients died after two years, 20 within the first six months, while others reportedly turned to prostitution and crime.
Since 1971, Britain has spent more than £200bn waging the war on drugs, according to the charity Transform Drug Policy. By any rational measure, it has not been a success. Police raids costing extortionate sums and taking months of planning rarely dent illegal supply for more than a matter of hours, police and crime commissioners have said. Drug gangs have become increasingly ruthless and exploitative in response, leaving them unrecognisable from those who first saw a profit to be made four decades ago.
Already rich from the trade in cities, crime groups now use thousands of vulnerable children and adults to pump drugs from major cities into rural areas in operations dubbed “county lines”. This drug money, the National Crime Agency estimates county lines operations are worth at least £500m, is then used to fuel other crimes, the rates of which are rising across England and Wales.

Heroin accounts for 90 per cent of the county lines problem and fuels organised crime more than any other drug, according to former undercover detective Woods. He recalled meeting a “cheeky 16-year-old” gang member while undercover in Leicester. Six months later the boy was a “terrifying 17-year-old” because “that’s what the trade made him ... the most successful drug dealers are the ones who are most intimidating because they don’t get grassed up. By policing drugs we’ve created this Darwinian situation and the personalities of our young men are being changed as a result.”
Drug users are simply “caught in the crossfire in this war”. Woods is now chairman of Law Enforcement Action Partnership UK, which advocates an end to the war on drugs. “Policing never reduces demand,” he explained. “It never reduces the size of the market and it never can because this is a health issue.”
While heroin addiction is now less widespread than during the infamous Trainspotting decade, Britain has an estimated 330,445 high-risk opioid users – more than any other European country. The UK is experiencing a drug deaths crisis, and in 2017 accounted for a third of Europe’s total. Heroin deaths show no sign of abating: already at record levels, there was a 16 per cent spike in 2018.
It’s often the most vulnerable in our society who are affected. Two-thirds of “problematic” heroin users are thought to be self-medicating for childhood abuse or trauma, while deprivation goes hand in hand with the drug’s prevalence. The areas hit hardest by drug deaths are generally coastal towns, often suffering the worst levels of poverty, unemployment and homelessness.
While some people tell us they became homeless as a result of their struggles with drug use, others use drugs to help them cope with the trauma of life on the streets
Rough sleeping has increased by 165 per cent since 2010 and the number of homeless people using and being killed by drugs is rising sharply, according to charity St Mungo’s. “While some people tell us they became homeless as a result of their struggles with drug use, others use drugs to help them cope with the trauma of life on the streets,” says Andy Mills, of St Mungo’s. “For the people we work with, drug use is often bound up with mental health problems and traumatic experiences from their past, which may also have contributed to their homelessness.”
Many users end up in jail, which proves no barrier to maintaining a habit. Woods asserts that prison can become a downwards spiral for drug users, “piling trauma on top of trauma” while accruing drug debts that have to be paid for by crime on the outside.
The Chief Inspector of Prisons, Peter Clarke, stated in his latest annual report that “the ready availability of drugs in too many of our prisons sits behind much of the violence. We are regularly told how easy it is to get hold of illicit drugs and of the shockingly high numbers who acquire a drug habit while they are detained.” Forty-two per cent of women and 28 per cent of men surveyed had a drug problem on entering prison.
There are many factors at play in the current crisis. A combination of increased opium production in Afghanistan and less border seizures in the UK has fuelled a resurgence in high purity heroin. This is often consumed alongside crack cocaine or tranquillisers by an ageing population of users, such as those who developed a habit in the 1980s and 1990s, and for whom underlying health complications can create a lethal cocktail.
After a decade of austerity, the budgets of most lifeline services (social, police) have been slashed. In the past year alone, nearly 60 per cent of local authorities cut budgets for addiction services, amid government cuts to public health grants.
These cuts came as responsibility for providing addiction services was passed to local authorities in 2012. Reduced funding led some areas to financially incentivise a focus on abstinence, pushing out the treatment of many more entrenched users who relied on regular methadone prescription to help curb their street drug use.
As a result, there is now a deafening clamour of voices – health experts, former addicts, law enforcement agents and politicians – arguing that by eroding existing treatment methods and failing to explore other viable solutions, our country’s drug policy has exacerbated and fuelled the current crisis. As our own history shows, it doesn’t have to be this way.
A new approach
While the UK’s first heroin crisis spiralled out of control and the British System was largely forgotten, other countries looked to our history for a potential solution. In 1989, Swiss researchers visited Dr John Marks’ clinic in Merseyside and were reportedly impressed by the health and wellbeing of his patients. Five years later, Switzerland created the first heroin-assisted treatment (HAT) centre.
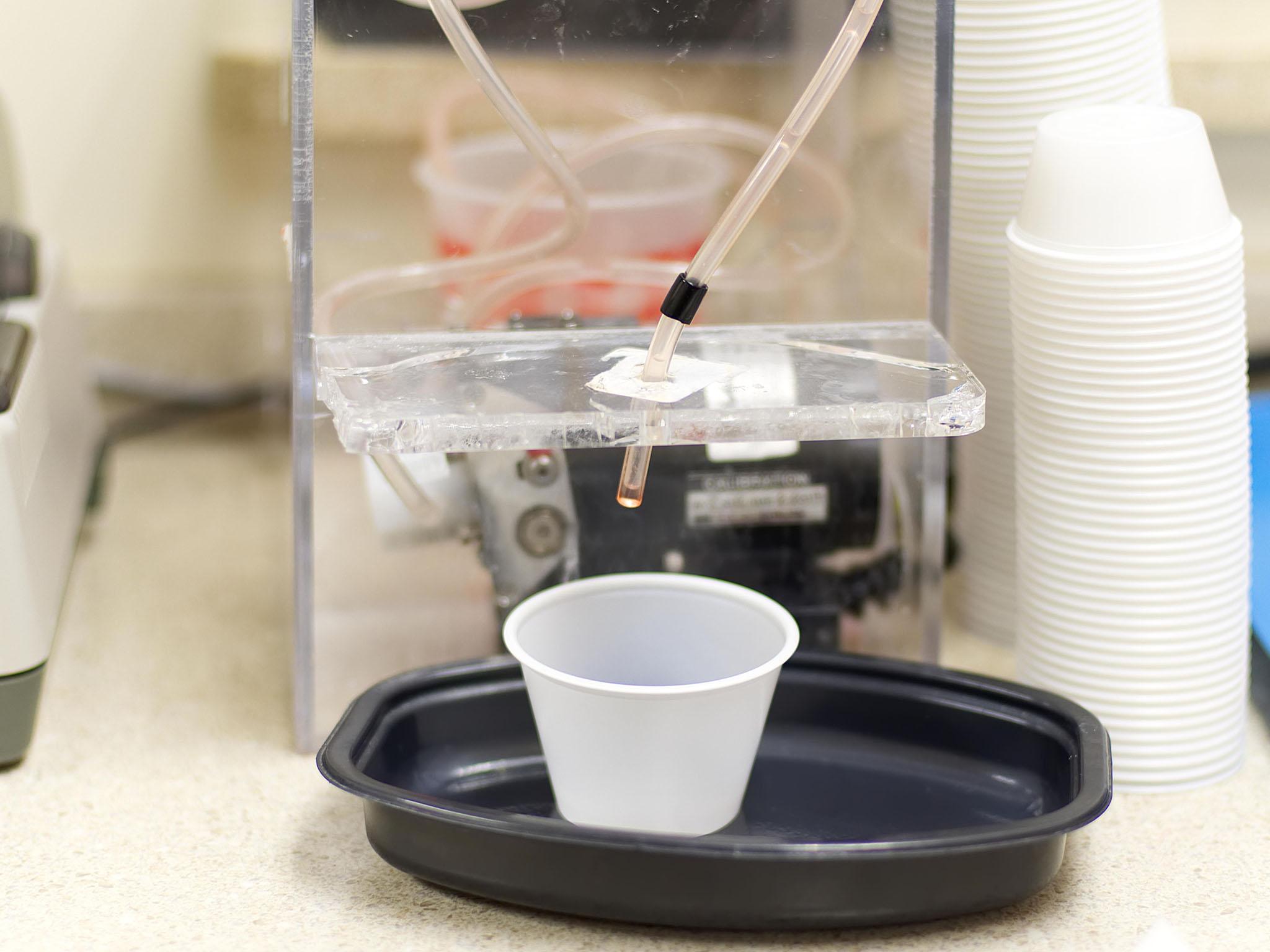
Expanding upon the British System’s basic premise of take-home heroin, the drug (diamorphine) is prescribed two to three times daily by specialist doctors and self-administered in the presence of healthcare professionals. The treatment is available only to those for whom two less intensive treatments, methadone and buprenorphine, have been unsuccessful – around 10 per cent of users. This cohort, now catered for by the government, used to account for 50 per cent of the country’s entire heroin market.
Since its introduction, Switzerland has seen street prostitution eliminated, drug deaths drop by two-thirds and burglary reduced by 50 per cent.
County Durham’s Police and Crime Commissioner Ron Hogg visited Switzerland in 2017 and has advocated strongly for the nationwide roll-out of HAT ever since. “The most striking thing I noticed was the difference in the life of a heroin addict in Switzerland and one in County Durham,” Mr Hogg said. He recalled meeting Chantal, 53, in Switzerland, who has taken heroin on and off for 30 years. She told him that “the clinic has given her stability, allowing her to rebuild her life, and see her daughter regularly. Contrast this to Lisa, a heroin addict in County Durham, who leads a life of crime, whose only thoughts are where to get money for her next fix.”
In sharp contradiction to the “shooting gallery” imagery often employed in relation to HAT, he describes the inconspicuous clinic as having “the feel of a dental surgery”, and stressed the strict empirical approach taken in the programme’s development. The Swiss model evolved in line with results gathered through rigorous documentation, evaluation and public consultations, he explained.
Switzerland has seen street prostitution eliminated, drug deaths drop by two-thirds and burglary reduced by 50 per cent. Anyone we spoke to in Switzerland, be that police officers, social workers, treatment centre nurses, business owners had no criticism to make
“Anyone we spoke to in Switzerland, be that police officers, social workers, treatment centre nurses, business owners had no criticism to make,” he said. This assessment holds up. In a 2008 referendum held on HAT by the right-wing Swiss People’s Party, 68 per cent of the country voted to keep it.
Germany, Holland, Denmark and Belgium have already followed suit. In the years leading up to 2009, it was trialled successfully in Darlington, Brighton and London, where lead researcher John Strang concluded the “impressive” results had shown major reductions in the use of street heroin: a success rate of 88 per cent compared to oral methadone (66 per cent) and its less common injectable counterpart (81 per cent).
Dr Strang recommended HAT be made available for selected heroin users across the UK, as the government had pledged in its 2008 Drug Strategy on condition of the trials’ success. Three post-trial pilot programmes were opened in 2012, but despite the government’s pledge, central funding was removed in 2015 and all of them were closed. While, if anything, public support for HAT has since grown, no new centres have been opened – until now.
In Scotland, which in 2018 had more drug deaths per capita than any other European country and an opioid-ravaged United States, health professionals have undertaken years of careful planning to open the country’s first clinic. It is set to open in Glasgow later this year, initiated partly in response to the highest rise in new drug-related HIV diagnoses in the city since 1985.
Ronnie Cowan, MP for neighbouring Inverclyde and vice-chair of the All-Party Parliamentary Group on Drug Policy Reform, is optimistic about the new centre: “The outcome is that no one dies from an overdose, crime is reduced, the surrounding area is not blighted by the detritus of needles and bloodied wet wipes.”

Users will also have on-site access to peer support, primary care, HIV treatment and advice services on issues such as housing and welfare rights. Mr Cowan believes it’s this “provision of a wider service and the availability of healthcare, welfare and medical professionals to work together” that sets HAT apart from existing opioid substitution methods such as methadone and buprenorphine.
For those the new clinic aims to help, being in treatment and in a position to form personal bonds with health professionals can be the difference between life and death. Currently, only 42 per cent of people using opioids in the UK are in this position. Around 10 per cent of Glasgow’s estimated 5,500 heroin users publicly inject drugs in the city centre – a group for whom homelessness, hospital admissions, jail-time and overdoses are common. It is largely this vulnerable, high-risk group that will be eligible for HAT. If Switzerland’s figures are anything to go by, providing them with legal heroin could put a dent in around 50 per cent of the UK’s total heroin market. Plans to get HAT centres off the ground in Ron Hogg’s County Durham and in nearby Cleveland are also under way.
Around 10 per cent of Glasgow’s estimated 5,500 heroin users publicly inject drugs in the city centre – a group for whom homelessness, hospital admissions, jail-time and overdoses are common
Not everyone is happy about the new approach. Residents have complained that the clinic could become a hub for drug-related crime and dealing. However, various studies of drug consumption rooms and HAT centres have shown not only no increase in crime, but a long-term decrease. Critics also say that by prescribing heroin, users could be stuck on the drug for years with little incentive to seek an abstinence-based recovery. Conservative MSP Adam Tomkins wrote in April: “From the addict’s perspective … they are reasons not to quit, reasons to delay for yet longer the difficult and terrifying task of taking those first steps towards recovery.”
But this argument is one that puts drug users at risk. In the 1980s, UK-based doctors pioneered a philosophy that became known as “harm reduction”, pragmatically placing a focus on preventing harm, rather than solely aiming to prevent drug use outright. It’s since spread around the world.
Many in the UK now insist that putting the idea of abstinence and harm reduction at odds with each other is a deadly mistake, and experts and drug users spoken to for this article believe that the government’s 2010 Drug Strategy, which had this effect, has contributed to the rise in drugs deaths seen ever since.
“For addiction behaviours, the aim is not to engage in abstinence-based recovery but to have a better life,” explained Dr Rita Manghi, deputy chief medical officer at the University Hospital of Switzerland. Abstinence is a significant part of the Swiss HAT model, however. Dr Manghi reports that at the Geneva clinic, one-third of its patients take no drugs at all. “It works!” Dr Manghi assures me, and according to Dr Strang, a similar result was seen in Britain’s pilot centres in just three years.
For someone who has been at the sharp end of addiction, the new approach cannot come soon enough. Rachael Keogh began smoking heroin aged 13 and injecting at 15 before nearly losing both arms to her addiction. She spent a decade in and out of jail from the age of 15, after resorting to theft and shoplifting to fund her habit.
“I was too young to be recognised as an addict but old enough to be sent to an older women’s prison, with drugs readily available and exposure to things no 15-year-old should ever have to see and that was it,” said Ms Keogh, who documented these experiences in her memoir, Dying to Survive.
“The worst thing that could happen, happened. I was gone after that. It wasn’t a deterrent in any way because my addiction was driving my actions. If I had been seen as a sick person in need of help at 15 and given HAT in a safe environment and maybe weaned off drugs then I might have had a chance.”
“Simple but radical shifts in how we as a society view drug users are the first step in dealing with the heroin problem. HAT would eradicate the shame for the drug user and make them feel like they are been given a real chance to get better by society.
It would take heroin off the black market and give drug users a chance to access their treatment in a safe environment without the fear of been robbed, threatened or hurt
“It would take heroin off the black market and give drug users a chance to access their treatment in a safe environment without the fear of been robbed, threatened or hurt. Part of the reason most drug users cannot become drug free is because of the lifestyle attached to it. The getting, using and finding ways to take drugs. The associates and drug dens are a prison in and of themselves. If HAT was offered it would take all of that away and give drug users a chance to breathe and focus on the next step of their recovery.”
Giving people time to work through underlying issues in a safe environment is a huge benefit of HAT, and as shown by Switzerland’s abstinence figures, doesn’t de-incentivise people to eventually stop using drugs.
Prun Bijral, medical director at one of the UK’s largest drug treatment providers, Change Grow Live, has witnessed this firsthand while prescribing diamorphine under the British System: “I’ve seen people say ‘I’ve done what I needed to do, I’m now ready to move on, I’m now at a stage where I feel able to come off this medication because my life has changed, I’ve spent that time’.”
A new British system
For some, the current model of HAT is too restrictive. Given the UK’s unique history of take-home heroin prescribing, some feel we have the expertise to go further than the model adopted in Europe. As Dr Bijral puts it: ”We have experience in this country that others don’t of being able to manage diamorphine in the community.”
Patients will have to turn up to the clinic two or three times daily to receive their medication, which can make the treatment a hindrance further down the line, stopping them from holding down a job or potentially rebuilding broken bonds with family and friends. For Dr Bijral, and others who work in addiction services, HAT could work in tandem with the British System of old – once patients’ lives have stabilised via the clinic, they could start to receive take-home diamorphine.
“I wouldn’t be an advocate of saying diamorphine for everybody, but I would love to be in a position – and I’m sure many services would – where you could give a range of options that suited the individuals and through discussion with professionals were able to come up with the best treatment for them,” said Dr Bijral. But he adds: “Unless it’s specifically funded, it would be very hard to justify providing diamorphine treatment for one person if it meant not being able to provide treatment for tens of people.”

In its current form in Switzerland, heroin-assisted treatment costs between £10,900 and £17,500 per individual each year, but this is an expenditure compensated for by “significant savings to society”. The Home Office puts the social and economic costs of drug supply in Britain at £20bn – up by £9.3bn since 2013. Considering the claim that 90 per cent of county lines alone is about heroin supply, the implication of the drug’s role in this overall estimate is significant, and Public Health England estimates that heroin-related crime costs the state on average £26,000 a year per user.
While expensive to set up in the short-term, the longer term fiscal benefits of HAT are expected to be felt widely across society. Durham PCC Ron Hogg explained how a reduction in demand for illicit heroin via HAT could “make a huge difference to individuals, their families and the wider communities” by allowing a stretched police force to “focus on tackling the organised crime groups, the real criminal causing misery to society”, as well as modern slavery, child abuse and cyber-enabled crime.
However, funding for addiction services is already thin on the ground. The abolition of ring-fenced central grants in 2012 came as the government transferred sole responsibility for drug treatment to increasingly cash-strapped local governments, and has stretched services to dangerous levels. There are serious issues with access and waiting times for existing opioid treatments, while vital services like needle exchanges are also at risk due to decreased funds.
For many councils it’s simply impossible to create such programmes while existing treatments are so dangerously underfunded, meaning they are forced to choose one lifesaving treatment at the expense of another. Every single person asked about funding during the research for this article called for the re-instatement of ring-fenced central government grants, not just for HAT, but drug services as a whole.
The Home Office and Public Health England frequently attribute the rise in drug-related deaths to ageing, entrenched heroin users. It’s argued this defence employs a cynical veil of inevitability, intended to act as a get-out clause amid funding cuts and a heavily criticised “recovery“ agenda, but it remains true that older, entrenched users are highly at risk.
HAT is proven to be an effective treatment for many in this group where others have failed and, it’s widely believed that in conjunction with reinvestment in existing services, could play a key role in reversing the fortunes of some of the most vulnerable in our society.
“Heroin may be the most destructive and difficult drug but it’s certainly the easiest one to regulate and it’s the one that will have the biggest impact on society if we get to grips with it,” Woods said. “Even if people don’t care about the plight of somebody self-medicating with heroin to deal with childhood trauma, once it’s explained that this can significantly reduce crime like no other policy, they start to get it.
“Once you explain you’re taking this money away from gangsters by taking their business away from them, they really start to get it.”
This, he says, is the first step in that journey.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks