How eConsult is trying to make treating patients more effective
Medicine is based on getting information from the patient, the essence of eConsult is to ask the questions ahead of the consultation, Heather Martin discovers


Murray Ellender gave Mark Harmon a job. Murray needed help with then fledgling health-tech company eConsult, and Mark was “a junior senior doctor” in search of something to tide him over for a few months during a career break. “That was five years ago,” Murray tells me. Back then eConsult employed only five or six people. Mark is now chief strategy officer and eConsult is embedded in around 3,300 GP surgeries, has a reach of roughly 29 million patients, averages 1.2 million remote consultations a month, employs more than 100 people – one in five of whom are clinicians – and has trebled in value. It’s the world’s leading triage provider, pointing people to the right door of the NHS to access the treatment they need as promptly as possible.
“I overstayed my welcome,” Mark says, with a wry smile. But he has the X-factor. Maybe it’s innate, or maybe it comes from hanging around with Roger Federer during his seven years as a director of Nike, first running the performance division of apparel for Europe, the Middle East and Africa, then the UK sportswear division, “the second biggest business in the world for Nike, with a turnover of $450m. That was before I saw the light.”
What made him leave? “Life’s too short,” he says. “I’d achieved what I wanted to, and my values and perspectives had changed. I had two young kids. When my son was born he was quite ill. I spent a lot of time in hospital departments through the night, with a lot of time to think.”
Mark’s parents ran a hotel business in the Highlands, so he started out waiting at tables, but his grandparents were both medics, and he’d studied pharmacology at Edinburgh before rebelling and taking a job with M&S – their graduate salaries were top-notch and they offered around-the-world travel, but mainly it was because “they had free wine and sandwiches”. It was ideal training for Nike. Further down the road he turned his back on a trainee place at London’s St George’s Hospital. In those days his head ruled his heart. But when he had children, his heart kicked back in. “I wanted to learn more, so I could help my son. He was the catalyst.” He eventually qualified as an A&E doctor aged 42, the oldest in his cohort at King’s College London.
Too old, perhaps, to relish the peripatetic lifestyle of the junior doctor, with placements all over Kent that would take him away from his young family, which is when Murray came to the rescue. “It was always my intention to combine medicine with my commercial experience, and that’s why I found it so enlightening meeting Murray.”
For Murray, it was the reverse. He’s been a doctor for 22 years, and is now combining his medical experience with commerce. He too went to King’s, with the intention of working in A&E alongside his wife, until they both decided to become GPs in the naive hope of a social life. How did that go? “Working as a general practitioner is the purest form of medicine,” he says, “because it’s so broad. You meet new people with new problems every day.” It was sort of social, if you took a philosophical view. Having four children was sociable too.
If you have an emergency, it’s 999; if you have symptoms, it’s eConsult. You put in your symptoms, and this intelligent cortex computes your acuity and directs you accordingly
Murray describes eConsult as “a spin-out from the NHS”, born of both love and frustration: love for the NHS and all it stands for, and frustration at the way it was creaking at the seams, even before Covid. “We’d been banging this drum, saying there needs to be more digital in health care, and here’s what it should look like. It suddenly became incredibly useful during the pandemic, and we saw real acceleration.” Now his work as CEO takes up 90 per cent of his time.
Established in 2014, eConsult arose organically out of a south London surgery. Murray and his colleagues were frustrated with the model of general practice, “which had remained unchanged forever”. “To see a GP, you have to get on the phone and book an appointment, then we have to bring you into a building and sort something out. Like everyone, we knew technology held the key.” But video alone didn’t solve much, because you still needed 10 minutes with a doctor and 10 with a patient at the same time. There was no real efficiency saving. Plus, it might take three of those minutes to connect to the patient. You’ve lost a chunk of time just because the broadband’s rubbish.
“Medicine is mostly around taking a decent story from the patient. The essence of eConsult is to ask the questions ahead of the consultation. We gather information 24 hours a day, at the patient’s convenience.”
They picked 50 common conditions, designed the perfect set of questions for each, then pointed their patients to their website. Doctors could match the information to medical records and deal with many conditions remotely, but not only that: having advance information meant they could plan and prioritise, not least as regards in-person appointments. That was phase one. The basic principle? “You only bring into the building the people you need to bring into the building.”

Phase two was to take the knowledge and expertise garnered in phase one and drop it into a higher acuity setting, with the appropriate intelligent algorithms. Whereas the emphasis for a GP is to gather a full history, in A&E it’s about how quickly you can identify the sickest patients. “The only place you don’t have visibility of the patient is in the waiting room. Once they’re in the system, you know where they are, you know their condition, you know how they’re progressing.” According to Murray, the average time to see a triage nurse should be 20 minutes, but is currently well over an hour, often far longer. “If you’re septic and you sit for three hours, you’re 24 per cent more likely to die. Same with a heart attack. Nobody should ever die in our waiting room.” With eConsult, patients are immediately assigned to one of five categories, ranging from P1 (life-threatening emergency) to P5 (can be safely redirected somewhere else). “Within five minutes of a patient walking through the front door of the hospital, we know who they are, how sick they are and where they need to go.”
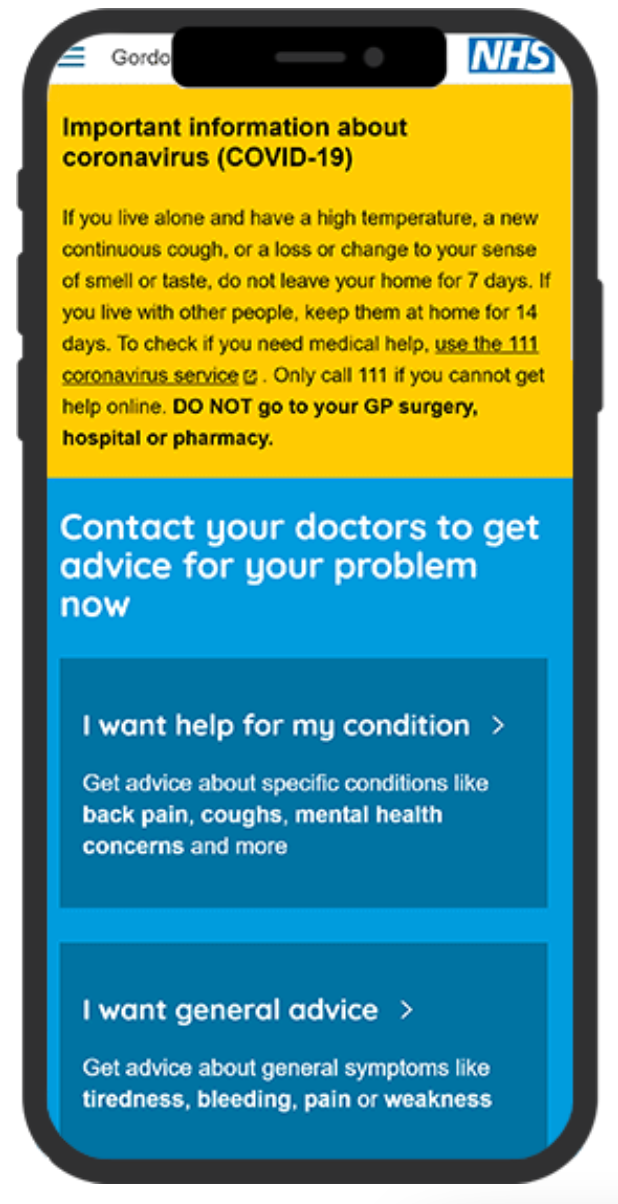
The aspiration is “to become a vernacular. If you have an emergency, it’s 999; if you have symptoms, it’s eConsult. You put in your symptoms, and this intelligent cortex computes your acuity, and directs you accordingly. The aim is to route patients from their own front door to the right door of the NHS, because at the moment people are turning up at the wrong door.” Mark describes the long-term goal as “joining the doors” between primary care, A&E and outpatients in an “integrated digital ecosystem”.
The eConsult USP lies in being clinically led, Murray says. “Most competitors are tech innovators coming into the medical market. We’re medical innovators in the tech space. We want to preserve the NHS and make it more sustainable.”
“We were first to market with online consultations,” Mark says, “first with A&E digital check-in, first with a virtual outpatients model.” Now they’re developing remote observations so a camera can take vital signs at the door. “We’re creating a wired community of clinical users. We’re constantly learning. Our product is updated every two weeks; it’s never finished. Yes, we need to be a successful business, but the key thing that gets us out of bed in the morning is actually sustaining the NHS, so it’s a better service, future-proofed, and still free for all.”
Conceived by Mark, eConsult even has an eLab modelled on Nike’s legendary Innovation Kitchen, where the best of the in-house team collaborate with the best external consultants to brainstorm improved models of health care. “That’s where we ask: what is the future going to be? Many minds are greater than one.”
Start-up costs were modest, says Murray. “We boot-strapped it for the first few years.” But as more players came to the market they began to seek external funding, mainly to strengthen the tech, and in 2020 secured £7m in an investment round. The more funding they attract, the better they can support the NHS.
Murray tells me a story. It’s about a young man who showed up at A&E one Saturday morning after a heavy night out. He was complaining of a headache. There was no queue: eConsult “has eliminated the queue”. Instead, there was a bank of iPads, ready and waiting, with questions tailored to pick out the headaches that matter most. One of them was: “Does it feel like you’ve been hit over the back of the head with a baseball bat?” The young man answered: “Yes.” This indicated a sudden onset headache, which is a symptom of a bleed on the brain. Because the question was asked within minutes of his arrival, they were able to flag him as urgent and get him transferred straight out to the specialist unit at King’s. It turned out he had a brain haemorrhage. “In the old days, the response would have been, ‘He’s just got a hangover. Stick him in the corner, he can wait’. He could have waited a long time to even be triaged.”
None of us likes waiting around to be seen. But it turns out it’s worse than mere inconvenience. “Taking a detailed history right at the start of the story makes the waiting room safe.”
As a kid Mark would go skiing every Sunday with his school. “If you can ski in Scotland you can ski anywhere, the conditions are so bad.” Murray used to row and do rock climbing. Now Mark cycles and Murray runs. Solitary pursuits, mostly, that free up headspace. “It’s what keeps us sane,” they agree. Mark is more measured, Murray more ebullient. They seem motivated by a sense of mission. But I’m still not sure about their social life.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments



Bookmark popover
Removed from bookmarks