‘I’d sell my soul to the devil just to get the help he needs’: How one family is struggling with schizophrenia
Promising athlete Aaron Dumsch’s downward spiral has taken everything from him. Such tragedy shows that the US must confront the flaws in its mental health system, says Abigail Jones

Your support helps us to tell the story
From reproductive rights to climate change to Big Tech, The Independent is on the ground when the story is developing. Whether it's investigating the financials of Elon Musk's pro-Trump PAC or producing our latest documentary, 'The A Word', which shines a light on the American women fighting for reproductive rights, we know how important it is to parse out the facts from the messaging.
At such a critical moment in US history, we need reporters on the ground. Your donation allows us to keep sending journalists to speak to both sides of the story.
The Independent is trusted by Americans across the entire political spectrum. And unlike many other quality news outlets, we choose not to lock Americans out of our reporting and analysis with paywalls. We believe quality journalism should be available to everyone, paid for by those who can afford it.
Your support makes all the difference.Alissa Dumsch flips through her high school yearbook, pausing on a photo of a hulking young man with sandy hair and a chiselled jaw. “There’s Aaron,” she says, pointing to her brother. “He was so good-looking.” She turns a few more pages. “Here he is at student council. I ran every year – and I lost every year,” she says, laughing. “He ran one year and, like, won by a landslide!”
We’re sitting in her home in Scarsdale, New York, along with her parents, Anita and Pat, and her sister, Amanda. Alissa’s husband quietly tapes hockey sticks in the corner while the youngest of their three boys, a toddler, waddles into the room with an oversized navy helmet teetering on his head.
Aaron is the only one missing. He knows we’re here though. His parents told him. And he knows about this article; he gave me permission to write it the first time we spoke by phone, in the autumn of 2018, when I explained what it would mean to share the story of his struggle with mental illness with a journalist and have his name and photo printed in a national magazine. “That would be awesome,” he said. As time went by, his family and I continued to check in to make sure he still felt that way.
Pat reaches towards the coffee table and picks up a scrapbook, titled “A Superstar’s Keepsake”, that Alissa made decades ago to commemorate Aaron’s accomplishments in high school. “Oh gosh, it makes you think,” he says, studying the pages as if they were Aaron himself. “Wish you could turn back time, go back to that day and relive some of these things.”
In 1990s Tucson, where football reigned and quarterbacks were king, Aaron Dumsch looked the part. He was a military brat who’d arrived at Sahuaro High School his sophomore year oozing natural talent. “He was a tall kid, with a rifle arm, and real smart. He had all the potential in the world,” recalls former Sahuaro football coach Howard Breinig.
During the final game of the 1994 season, Sahuaro’s senior starting quarterback injured his shoulder; Aaron, a junior, took over with less than a minute before halftime and his team trailing 21-20. He threw six passes in 37 seconds, giving Sahuaro a 27-21 lead at the half. Sahuaro won that game, and Aaron’s heroics continued soon after, at the Class 4A state championship. Sahuaro was down 17-9 with 1:27 left on the clock when he scored a touchdown and a two-point conversion, tying the game, earning his team a co-state championship and sending Breinig, who was retiring that very night, off with his first and only state title.
“I remember sitting in the stands – I still get teary-eyed thinking about it,” Alissa says. “We couldn’t believe it. We were so proud. He was so talented.”
The Dumsches could tell stories about Aaron’s exploits all day, but there are other tales, too, the kind his family would rather forget. Like the time he shoved a woman with a walker. Or the time he lay on the couch, watching the news coverage on 9/11 and laughing. “We’d lock our bedroom doors because we were afraid he’d come in and hurt us,” Anita says. “He could go into these rages where he would just scream and holler and push and hit.”
Protecting the mentally ill, you become mentally ill just trying to get it all together
Over the past 20 years, Aaron has spiralled from a high school star and an academic all-American on the Arizona State University football team to a ward of the state of Maryland. He has been captive not just to a schizophrenic brain but to a perfect storm of factors – underfunded treatment facilities, prisons and jails serving as de facto asylums, a lack of advancements in medication – that has made it generally harder for people with serious mental illnesses to get the help they need.
All the while, Anita has been at Aaron’s side, trying to care for her son while insulating her family – and the public – from his unpredictable behaviour. As she puts it, “Protecting the mentally ill, you become mentally ill just trying to get it all together.”

High school sweethearts from Michigan, Anita and Pat Dumsch married young and had Aaron in their early 20s. Alissa arrived 17 months later, Amanda three years after that. Anita was a secretary, and Pat worked at a factory, but life was a struggle until Pat joined the Air Force, training as a dental hygienist and moving his family to six states and Norway over the years.
Wherever the Dumsches landed, Aaron’s athletic talent shone. When he was 6, football scouts came to the Dumsch home in Wichita Falls, Texas, to persuade his parents to let him play. At 10, he made it to a state championship free-throw shooting contest. At 12, he was the starting pitcher on a Norwegian baseball team, leading it to the Little League World Series in Europe. In high school in Tucson, he quit baseball midseason, switched to track and won his first race wearing borrowed shoes. “Every sport at almost every stage in his life he excelled at. It was crazy stuff,” Anita says.
By senior year, Aaron’s star seemed unstoppable. As quarterback on the football team, he was a fixture on the local news. USA Today nominated him as an all-American high school athlete. But he was more than a jock. “He was a brainiac. Very sweet. A guy who could cry and wasn’t afraid to,” says Jennifer Carner, who dated Aaron for two years in high school and college. “But also he’d stick up for himself. He was this conundrum of a personality, but it was also what made him sexy.”
“He had this really genuine, warm spirit,” says Cara McCrain, a high school friend of Aaron’s and Alissa’s. “There was nothing he couldn’t do – in school, in [sports], have any girl he wanted. He was it.”
Graduating at the top of his class, Aaron was recruited by the Naval Academy but chose to attend Arizona State University (ASU); he’d had enough of military culture. He walked onto the football team at the end of his freshman year. (He had chosen not to play that autumn mostly on principle; ASU hadn’t formally recruited him.) Anita and Pat remember standing at the edge of a practice field at training camp when a player with long hair and flip-flops walked over and introduced himself. “I’m Pat Tillman,” they remember him saying. “I just want you to know you’ve got a really great guy here as a son and I’m gonna keep my eye out for him.” (Tillman, then a star on the ASU football team, later played for the Arizona Cardinals before famously enlisting in the Army after 9/11. He was killed by friendly fire in 2004.)
Aaron won awards for the highest grade-point average on the team and best offensive scout team player, and made the dean’s list twice. He had a girlfriend he thought he might marry. “He should have been CEO of a Forbes 500 company,” Breinig says, “or a professor at some big university.”
“He had this really genuine, warm spirit,” says McCrain. “There was nothing he couldn’t do – in school, in [sports], have any girl he wanted. He was it.”
Instead, everything unravelled. Aaron, certain that he’d receive a coveted football scholarship for his senior year, was gutted when it went to someone else. Anita calls that “the turning point”, the moment that “broke his spirit”. That autumn, he quit the team. He spent his days smoking cannabis. Soon, he began calling home with strange claims: His dorm room was bugged, or his toes were growing, or the TV was talking to him. He lost a car and a couple of bikes. “Our initial thought was, ‘Oh dear god, I think he’s on drugs’,” Anita says.
Once, Alissa recalls, he grabbed her arm in the car. “They’re watching me!” he whispered, his face full of fear. When she asked what he meant, he leaned in closer, glanced behind him and said, “The movie Varsity Blues. They stole my life.”
Two weeks before graduation in May 2000, Aaron threatened students in an ASU auditorium, raving that he was going to fight them and kill them. “I get this phone call. It’s basically, ‘He’s being expelled. You need to come get him,’” says Anita, who dropped everything and drove up to Tempe. “I get to his dorm room, which was an apartment he shared with a guy, and he was like, stoned. I mean, he was totally stoned,” she says. “I was just so mad.”
Anita took Aaron to meet with administrators, and as he sat there mumbling, acting “completely out of it”, she begged them to let him withdraw rather than expel him from school. “In that moment I’m thinking, ‘He has a life ahead of him! He’ll never get back into college!’” Anita says. The administrators acquiesced. By the end of the day, she’d loaded everything Aaron owned into her small Nissan Sentra. “I remember his bike was on the back of the car, hitting the trunk the whole time. I mean – ”, she covers her face with her hands. “I couldn’t even believe I was doing this.”
And so Aaron moved home. His parents were still convinced he was using drugs, but the truth was more alarming: Aaron was in the midst of his first psychotic break.
“The onset is so cruel,” says Steven Hyman, director of the Stanley Centre for Psychiatric Research at the Broad Institute of MIT and Harvard. He’s referring to the fact that schizophrenia typically strikes in the teens and twenties. “Family and society are just finishing their incredible fiscal, emotional, cognitive investment in the production of a wonderful person, and that person is snatched away.”
Fewer than 1 per cent of Americans have schizophrenia, though the rate is difficult to measure because the illness can be hard to diagnose and many population studies omit people who are institutionalised, incarcerated, do not speak English or are homeless, according to the National Alliance on Mental Illness (Nami). It is a severe mental illness affecting how a person thinks, feels and acts. In addition to delusions and hallucinations, symptoms can be as varied as a flat affect and lack of focus and motivation, disorganised thinking and speech, difficulty making decisions and expressing and managing emotions, and memory loss and other cognitive impairments. Some people hear voices and believe others are plotting against them.
Scientists don’t know exactly what causes schizophrenia because the brain is so complex. While some of the risk has to do with genetics, most people with schizophrenia don’t have a first-degree relative with the illness, though many have a family history of psychosis (suicide and substance abuse run in Aaron’s extended family). Environmental factors – such as stress, trauma, maternal malnutrition, and infection before birth and during childhood – can play a role. Evidence also shows that heavy cannabis use is a factor, especially among young people with a history of family psychosis, though this connection is controversial. For those who already have schizophrenia, cannabis can trigger psychotic episodes.
With effective treatment, some people with schizophrenia lead fulfilling lives, but there is no cure, and due to a variety of factors, people with schizophrenia (and other serious mental illnesses) die on average more than 25 years earlier than the general population. Schizophrenia also wreaks havoc on families, who can spend decades mourning a loved one who’s still living. Stigma makes an already dire situation worse.
It would be so much easier to say Aaron had brain cancer, because the empathy would be immediate. When I say, ‘My son is mentally ill with schizophrenia,’ it’s as if I said leprosy
“I used to hesitate to tell people about this disease,” Anita says. “It would be so much easier to say Aaron had brain cancer, because the empathy would be immediate. When I say, ‘my son is mentally ill with schizophrenia’, it’s as if I said leprosy.”
I first met Anita and Pat in the autumn of 2018 at their home in Bowie, Maryland. It was a week before Thanksgiving, and they had already erected not one but two towering Christmas trees. In the photographs scattered around the house, time seemed to stand still: there were Polaroids of Aaron, Alissa and Amanda sitting on Santa’s knee; pictures of the three kids at various graduations; framed photos of Aaron wearing his maroon-and-gold ASU football uniform.
“Remember the Palo Verde hospital he was in, in the psychiatric unit? We walk in there to see him – I’ll never forget this,” Anita said. “He shaved half his head – just half! And he had these goggles. These glasses. They were so thick, because his vision was so bad, because he was on these drugs ... with severe side effects, like tremors and blurred vision. I remember we walked out of there, and I was like, ‘oh my god’. And then we hit a cat going home. I had my very first – ” she paused. “It was this horrible panic attack. I wanted to run through the patio window. We had a pool in the backyard and I remember waking you up” – she looked at Pat – “and I said, ‘I have to have someone hold on to my hand’. I had overloaded.”
Anita admits she ignored the first time someone suggested that Aaron might have schizophrenia. It was the autumn of his senior year of college, and she’d arranged for him to see a psychiatrist near ASU, thinking he needed drug counselling, possibly even help with depression. “The doctor contacts me and says, ‘Your son has paranoid schizophrenia.’ I said, ‘what?!’ He said, ‘It’s a full-blown case ... My practice is full, but you have to get him help. Things are gonna get worse.’”
Anita didn’t believe him. How could this doctor, who’d met Aaron only once, know anything about her son? “I thought it was a hasty diagnosis. I thought, ‘Oh, I just got a bad doctor,’” she says. Aaron returned to school, and the Dumsches carried on with their lives, hoping their “good boy gone bad”, as Anita puts it, would soon find his way.
Nearly a year later, after Aaron had left ASU and moved home, Anita and Pat slowly began to realise the truth: That psychiatrist had been right – Aaron really was ill. They found themselves living at home with a son they hardly recognised. Aaron would say that he was dating Winona Ryder, or insist that he was a German shepherd, or claim to be African American. He’d sit in the hot tub in their backyard, arguing with voices no one else could hear. He would wander the streets and get into fights or steal his parents’ money. When neighbours threatened to call the police, they’d say, “go ahead”, overcome with relief. (Aaron calls many of these incidents “painful memories”. That he remembers most but not all of them is part of his illness.)
Anita and Pat felt paralysed. They knew very little about schizophrenia and had no one to turn to. With two daughters to send to college and a combined $65,000 (£49,700) annual income, they also had few resources to draw on. Because of military rules regarding dependent coverage, Aaron lost his health insurance once he left ASU. Anita spent three years petitioning the Air Force to restore dependent coverage, then another two applying for social security disability benefits, including Medicare. She also applied for Medicaid for Aaron so that he’d be eligible for food stamps and group home and community programmes.
During these first few years, Anita and Pat – but mostly Anita – cared for Aaron on their own, managing his symptoms, traipsing after him at all hours of the day and night, searching for a cure. It was what she calls her “we can fix this” stage. “We were angry and mad and [would say] ‘straighten up’ and ‘why are you doing this?’ We didn’t realise the gravity of what he was in,” Anita says. “I really thought he’d come back and it was just going to take some really strong, tough love and restrictions.”
Sometimes they’d leave him in jail for a night, or bring him to a shelter. Once, he racked up $2,000 (£1,500) in hotel expenses. “Pat and I dropped him off at so many homes and halfway houses and crisis centres and, actually, bus stops. Things a parent shouldn’t ever have to do for their child,” Anita says. “I can’t tell you how many nights we drove around looking for him, whether it was in Arizona or Maryland or in DC or – ” she chuckles. “It would be hours and hours, and then we’d find him or we didn’t find him, and then we’d come home and go to work the next day. It was such a bizarre routine.”
The initial years of Aaron’s illness were especially painful for Alissa and Amanda, who were trying to make their way into adulthood with a storm hovering at home. Alissa developed an eating disorder while at Wellesley, but Aaron’s illness overshadowed it. “I didn’t get the help I would have had he not been sick,” she says. It took her 13 years to recover. After graduating in 2001, she moved in with her parents to help care for Aaron, but the arrangement barely lasted a year. “Our unit was unravelling,” Alissa says. “You almost wanted to hole up and pretend that life wasn’t happening around you.”
There was a flicker of hope in 2002, when Aaron, now 25, enrolled at the University of Arizona in Tucson and moved into an apartment near campus. His medications seemed to be working. He walked onto the Division I basketball team (but was disqualified before he could play because his years of eligibility had expired). For a brief moment, everyone could breathe again.
That autumn, Anita, who had been working as a secretary for the Air Force chaplaincy, was offered a promotion that would mean relocating to the Washington DC area. Aaron was seemingly settled, Alissa was living in New York and Amanda was at the University of San Diego. Pat, who had retired from the Air Force after 20 years of service, moved with Anita to Maryland.
Their respite was short-lived. Aaron’s landlord evicted him for smoking, bothering neighbours and panhandling. By Christmas, he’d flunked out of school and moved in with his parents. And so the Dumsches were back to the earlier pattern of trying to manage Aaron, knowing full well they couldn’t manage him at all.
The Dumsches clung to family life as they’d known it, taking Aaron to church, to the theater, on vacations. Disaster followed everywhere. During one stay at a hotel, Anita woke up in the middle of the night and realised that Aaron had disappeared, only to find him outdoors, doing drugs with some guy. After Alissa moved to New York, Aaron visited a few times. “All of a sudden he would just be gone,” she says. “And then you realise your neighbour is calling the cops because there’s some weird guy standing out front, and it’s my brother, spewing stuff outside your door.”
Friends and relatives told Anita to kick him out, or to watch A Beautiful Mind (about John Nash, the Nobel Prize-winning mathematician with schizophrenia) and Sybil (about a woman with an entirely different mental illness), as if those movies held some secret solution. “After seven years reliving the same thing over and over again, with the same results, I finally got to that point of accepting,” Anita says of Aaron’s illness. “Let’s stop trying to figure out why and how this happened. Let’s now try to keep him alive.”
By this point, Anita had already become the quarterback for Aaron’s care, calling doctors, navigating insurance companies, seeking out treatment programmes, managing his behaviour. Today, asking Anita to recount which group home or outpatient program Aaron tried when, or what each one focused on, is futile. They all blend together. “It’s a different city, different group home, different case manager. It could be the same city but a different home. I can’t even remember them all,” she says. “I have boxes of documents of every place. I just kept saving them. I didn’t know what I needed anymore.”
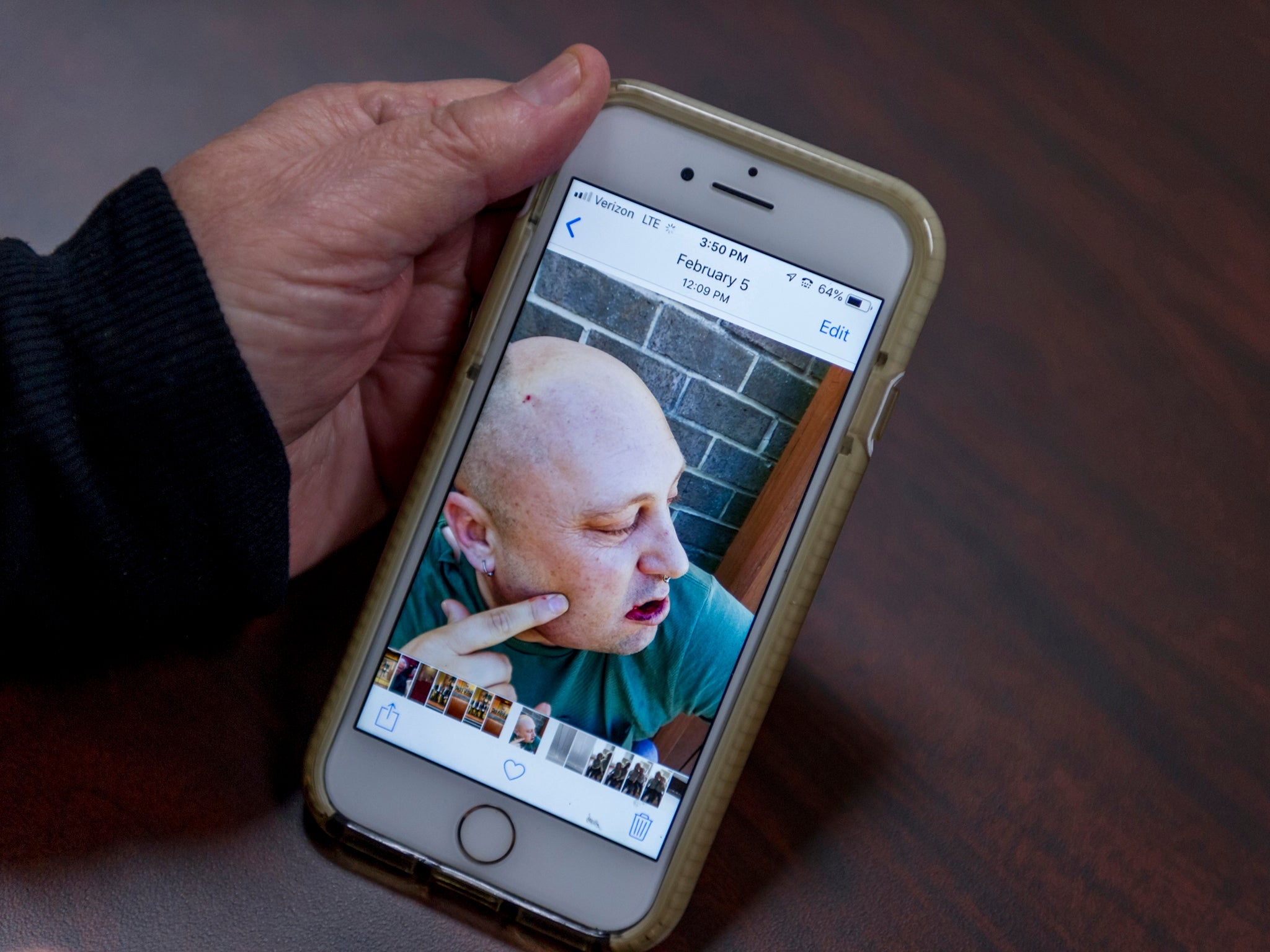
When I visited the Dumsches in Bowie, Maryland, in 2018, Anita drove me past a few of the programmes Aaron had tried. One was a group home on a quiet street, nestled amid two-story rowhouses. “It’s kind of this camouflage. It doesn’t look that bad until you open the door,” she said, showing me photos on her smartphone of broken windows, piles of garbage, a filthy bathroom and mattresses on the floor.
I’m letting you know that we’re putting him on the next plane. He’s going to get killed here
Another program convinced her that she should give Aaron more freedom, not less. “You can’t coddle him,” Anita remembers the psychiatrist saying. That advice proved nearly fatal when Aaron said that he wanted to go to Jamaica, and Anita reluctantly agreed. Within a week, she received a call from a woman at Aaron’s hostel. “She goes, ‘I’m letting you know that we’re putting him on the next plane. He’s going to get killed here,’” Anita says. “He was in really bad areas of Jamaica. She told me someone had a gun on him. He was asking to buy cannabis.”
As time passed, Anita and Pat came to realise that they needed a long-term solution for Aaron. They wouldn’t be around forever, and they vowed not to burden their daughters with his care. “It would destroy their lives,” Anita says. But where could he go? Emergency rooms typically sent him home as too high-functioning, and when they did admit him, he ended up in a mental health ward or in a behavioural health hospital for a few days to two weeks, which was never enough time to stabilise him. Insurance wouldn’t cover a longer stay. The Dumsches tried psychiatrists who visited the house and drop-off day programmes. Medication alone wasn’t a long-term solution; Anita often found Aaron’s pills in the toilet, inside his shoes or on the driveway. She even wrote letters to Oprah Winfrey and Dr Phil, begging for guidance. (They never responded.) “You’re just hoping for a miracle,” Anita says. “I’d sell my soul to the devil just to get the help I thought he needed.”

People with serious mental illnesses make up a third of the US homeless population, 20 per cent of jail inmates and 15 per cent of state prisoners, according to the Treatment Advocacy Centre (TAC), a nonprofit organisation working to improve health care and laws for those with severe mental illness. And the groundwork for this situation was laid long ago.
In the mid-19th century, teacher, author and activist Dorothea Dix championed the humane treatment of the mentally ill, establishing or expanding more than 30 mental hospitals nationwide and launching a movement for mental healthcare reform. A century later, state hospitals were overrun, understaffed and poorly funded, filled with patients living in often abhorrent conditions. With the discovery of new antipsychotic drugs, an effort began to empty out state psychiatric hospitals, sparking a historic shift to community-based care that was buoyed by the Kennedy administration’s 1963 Community Mental Health Act, which funded public and nonprofit community mental health centres (CMHCs), as well as the advent of Medicaid.
Between 1955 and 1994, the number of mentally ill patients in public hospitals fell from nearly 560,000 to 71,000, according to E Fuller Torrey, a psychiatrist and schizophrenia researcher who founded the TAC. Today, he puts that number at 35,000. While deinstitutionalisation succeeded in emptying out overcrowded state hospitals, the planned shift to community-based care was inadequately funded and staffed. CMHCs were supposed to be a lifeline for those with severe mental illnesses, but many catered to people with more “manageable” problems – only 4 to 7 per cent of CMHC patients came from state hospitals in the beginning, and as time went by, that number dropped, even though hospital admissions increased in the same period. In 1981, the Reagan administration turned federal funds reserved for CMHCs into block grants, giving states discretion on how to spend their dollars – and permission to ignore the federal model of care designed under Kennedy.
Some experts charge that CMHCs continue to focus on people with less severe problems, leaving individuals like Aaron to flounder. “It’s much easier to serve someone with mild depression or mild anxiety disorder who’s willing and able and wants to come to therapy sessions,” says Elinore McCance-Katz, assistant secretary of mental health and substance use at the Department of Health and Human Services, who leads the Substance Abuse and Mental Health Services Administration. CMHCs “need to do more to serve the most seriously ill, and they’re not doing that job right now. And states need to take care of people who are homeless, on the streets, psychotic, hungry, cold, physically ill and mentally ill. This is the US. Shame on us for not doing a better job.”
“I’ve sent a million emails. I’ve taken photos of the facilities. I’ve questioned how staff members are trained,” Anita says. “I’ve done all this because I don’t want to be the mother on TV being asked, ‘why didn’t you get him help?’”
Some people with schizophrenia lack insight into their illness and can’t or won’t seek treatment on their own. That’s Aaron. For such people, Torrey argues, Maryland “is one of the last states you want to be living in”. That’s because it’s one of three states without a law for assisted outpatient treatment, or AOT, which provides community mental health services under a civil court order for people with serious mental illness who have a history of refusing or struggling to follow treatment.
Studies have shown that AOT, if adequately funded, can reduce homelessness, hospitalisation and incarceration. Yet some critics argue that it violates patient civil liberties. Others believe there are more effective approaches to treatment than forcing compliance. “Part of the reason Maryland hasn’t gone down this road is there is a terrific working alliance between folks who receive services, the provider community and the department of mental health,” says Lawrence Fitch, former forensic director in Maryland’s public mental health system, who now teaches mental health law at the University of Maryland School of Law. “They work together to reduce stigma and try to encourage services that reach out to people. The goal is to make it attractive enough so people will want to receive services.”
Of course, the quality of that care often depends on local resources. “Aaron’s day program consisted of some groups but mostly hanging outside, smoking,” Anita says. Once, she tells me, he landed in a group home where he was mugged and had a gun pulled on him.
Another barrier to care is the number of patients at state hospitals who have a mental illness and are involved in the criminal justice system, known as forensic patients. Maryland has five state psychiatric hospitals, and court-ordered patients occupy most of these beds – 90 to 95 per cent at one facility, 60 to 75 per cent at the other four, according to the Maryland Department of Health. Forensic patients often stay for long periods, so it’s no wonder that Aaron – whose frequent admissions generally were not court-ordered – kept getting sent home.
All that changed over Christmas in 2006. That’s when Aaron finally “broke into the legal system”, as Anita puts it. He’d recently started dating a woman he’d met while at a doctor’s appointment. A few months into their relationship, she called Anita and Pat late at night and said that Aaron had hit her. Instead of trying to talk her out of pressing charges, they drove her to the police station so she could file a restraining order against him. Weeks later, the police showed up at their house with a warrant for his arrest, pulled him out of the shower and handcuffed him. “I was petrified they were going to shoot him,” says Amanda, who was home at the time. “I thought, he’s gonna say something or lash out, and they’re going to overreact. I was angry, but then, I was also relieved he was going.”
Aaron was taken to a local jail, then moved to Springfield Hospital Centre for evaluation. He didn’t leave for more than two years. When he finally did, it was under conditional release: He had to agree to take his medication, attend outpatient treatment, abstain from drugs and avoid altercations with the law for the next five years. If he broke any of these conditions, he’d go back to Springfield. This was the safety net Anita had been searching for. “We told him, ‘It’s not gonna be forever,’” she says. “In my head I was like, ‘if it is forever, he’s in the [hospital] system.’ Once you’re out, you can’t get back in unless you’re back in jail; I didn’t want him in jail. He’d be killed in jail.”
So far, Aaron has been released from Springfield three times in 13 years – and broken his conditional release each time. His current stay began in March 2018, after he hit a worker at his group home. For several months leading up to that incident, he’d been going off the rails during car rides with Anita, staring at strangers through the window and yelling, “I’m gonna f*** that person up!” and “That person’s a little b****** that needs to get kicked!” (Asked if he remembers those incidents, Aaron replied: “I feel so bad. When I was in high school, I always did the right thing. I got away from what made me a good person.”) Anita would contact the people involved in her son’s care – the counsellor at his group home, case managers – and explain that he was a danger to himself and others. But it would take months to get him into a more controlled environment.
Then, in early February 2018, Aaron got into a fight with the staffer at his group home. Despite a court order to admit him to a hospital, he was released within 12 hours, then sent to a crisis centre before being transferred back to Springfield. A week after this incident, one of the deadliest school shootings in American history unfolded in Parkland, Florida, when a 19-year-old man killed 17 people at a high school. That’s when US president Donald Trump issued a tweet that nearly broke Anita: “So many signs that the Florida shooter was mentally disturbed, even expelled from school for bad and erratic behaviour. Neighbours and classmates knew he was a big problem. Must always report such instances to authorities, again and again!”
I think if some of my teammates and coaches were to find out what happened to me, I think they’d be upset. There’s no way I should have gone through this
“I went berserk,” Anita says of the moment she read the tweet and realised that the president of the United States was essentially blaming those tragic deaths on the shooter’s family. “I was like, Oh my god! Nobody knows what I’ve gone through for the past 20 years. It was a direct hit as a family member that has alerted authorities more times than I can remember, only to be shut down, dismissed or ignored.”
One of the gravest misconceptions about people with serious mental illness is that they’re all dangerous. This refrain often surfaces after mass shootings, and yet most individuals with schizophrenia are more likely to be victims of violence than perpetrators, research shows. Aaron, of course, does have bouts of aggression, which is why Anita has worked so hard to contain his behaviour. “I’ve sent a million emails. I’ve taken photos of the facilities. I’ve questioned how staff members are trained,” she says. “I’ve done all this because I don’t want to be the mother on TV being asked, ‘Why didn’t you get him help?’”
The Dumsches know all too well that speedy access to leading treatments is harder than it should be. Nor is high-quality care a panacea; even if doctors found cures that eliminated active psychotic and major mood disorders, violent acts in general would decrease by just 4 per cent, according to Jeffrey Swanson, a professor in psychiatry and behavioural sciences at the Duke University School of Medicine. Yet a small number of people with serious mental illness do commit violent acts, and most of them are untreated or inadequately treated. That’s why, every day that Aaron isn’t safely at home or in a facility, Anita is terrified that he might hurt himself. Or someone else.
“I would love nothing more for Aaron than to come back home,” says Pat. “I miss the kid. I’d like to see him get some kind of a life again. He never will at this hospital. Again, it’s one of those situations where if he were to come home and he goes into these bizarre moments ...” He trails off, remembering the time Aaron punched him in the head twice, almost knocking him out.
“I’m not sure what’s gonna happen with me, Mom,” Aaron says. Anita leans forward. “Something will happen. Something always happens. We’ll just have to – ” she pauses. “Do the best we can.”
Not all stories of schizophrenia unfold like Aaron’s. Brandon Staglin had his first psychotic break in 1990, the summer after his freshman year at Dartmouth. “I was trying to fall asleep,” he says, “and all of a sudden, I felt like half myself had vanished – the right half of my head felt totally different. Like my soul had vanished. I tried to call back thoughts of my girlfriend, family, friends. None sparked any affection in me. It was terrifying.”
A few days later, Staglin checked himself into a psychiatric hospital in Walnut Creek, California. His parents, who had been travelling in Europe, rushed home and sprang into action. They had means and contacts, doctors they could call to help them find the best care for their son. And they were lucky. As Staglin puts it, “I had enough insight to realise something was wrong with me”.
Within three months, Staglin was on clozapine (which for decades has been the standard drug for treating schizophrenia; it hasn’t worked for Aaron). He was also in therapy, auditing classes at the University of California at Berkeley and volunteering at the Oakland Zoo. This multipronged approach was rare at the time, but it’s now considered the leading edge in treatment: coordinated speciality care (CSC). Based on years of research and a multisite National Institute of Mental Health study, CSC connects young people at the onset of psychosis with specialised wraparound services – like personalised medication management, psychotherapy, family education, work and education services, and case management – to help them keep their lives on track.
“Globally, we are aspiring to no more than three months of untreated psychosis, but ultimately we want to identify people who are at risk before onset and try to prevent the development of psychosis,” says Lisa Dixon, a psychiatrist who directs the Centre for Practice Innovations at the New York State Psychiatric Institute and leads OnTrackNY, a coordinated speciality care program delivering early intervention services to young New Yorkers. “We don’t have a cure for schizophrenia, but [CSC is] helping people cope with what happens to them, not sending them back into failing situations.”
According to a 2018 study, there are about 270 speciality care programmes in the US, reaching just over 7,000 people. But, says Dixon, this is still not enough.
A similar treatment model, assertive community treatment (ACT), connects individuals with serious mental illness with multidisciplinary support teams that help them navigate treatment. While studies show that ACT has reduced hospitalisations and arrests and improved quality of life for people with the most severe symptoms of mental illness, only 13 per cent of mental health facilities offer ACT services, according to a 2019 study.
Staglin offers a glimpse of just how powerful early intervention can be. After a year of treatment, he returned to Dartmouth, graduated with honours and landed a job in aerospace engineering. He had a relapse in his twenties but today lives in Napa, California, with his wife and runs One Mind, a family nonprofit dedicated to furthering brain research.
Though CSC may be the most exciting development in the field today, it won’t help people who have been living with schizophrenia for many years. And yet, while scientists have not figured out how to turn the Aarons of the world into the Brandons, Kenneth Dudek, senior adviser and former president of Fountain House, a leading community-based mental health model, has hope. “We shouldn’t be writing off 40-year-old people as dead. I have 50 examples that would counter that. Aaron should be here,” he says, referring to Fountain House, where people with schizophrenia and other serious mental illnesses gather, learn and work together in a sort of self-sufficient village. There are more than 300 programmes based on Fountain House around the world. “If you offer the right kind of support over a long period of time, people will have much better lives. They can have a real life,” Dudek says. “Chances of Aaron getting back to where he was is maybe not possible, but he could have his own apartment, a job, a relationship – those could happen as long as he starts to deal with his illness.

The drive north from Bowie to Sykesville, Maryland, is unremarkable – long stretches of leafless trees, dirty snow banks and suburban strip malls. Anita has gotten used to the monotony. She makes this hour-long trek every weekend, usually with Pat, to visit Aaron. It’s late November 2018, and sleet hits the windshield as Anita turns down the long, narrow road leading to the facility. Majestic brick buildings in varying states of decay rise up from the snowy fields. Scores of black vultures sit motionless on a fence. “This is the path to nothing,” Anita says.
A regional psychiatric facility operated by the state of Maryland, Springfield Hospital Centre opened in 1896 and once housed 4,000 patients on its 1,300 acres. Today, it’s a relic of the deinstitutionalisation movement. Only about half its buildings are in use.
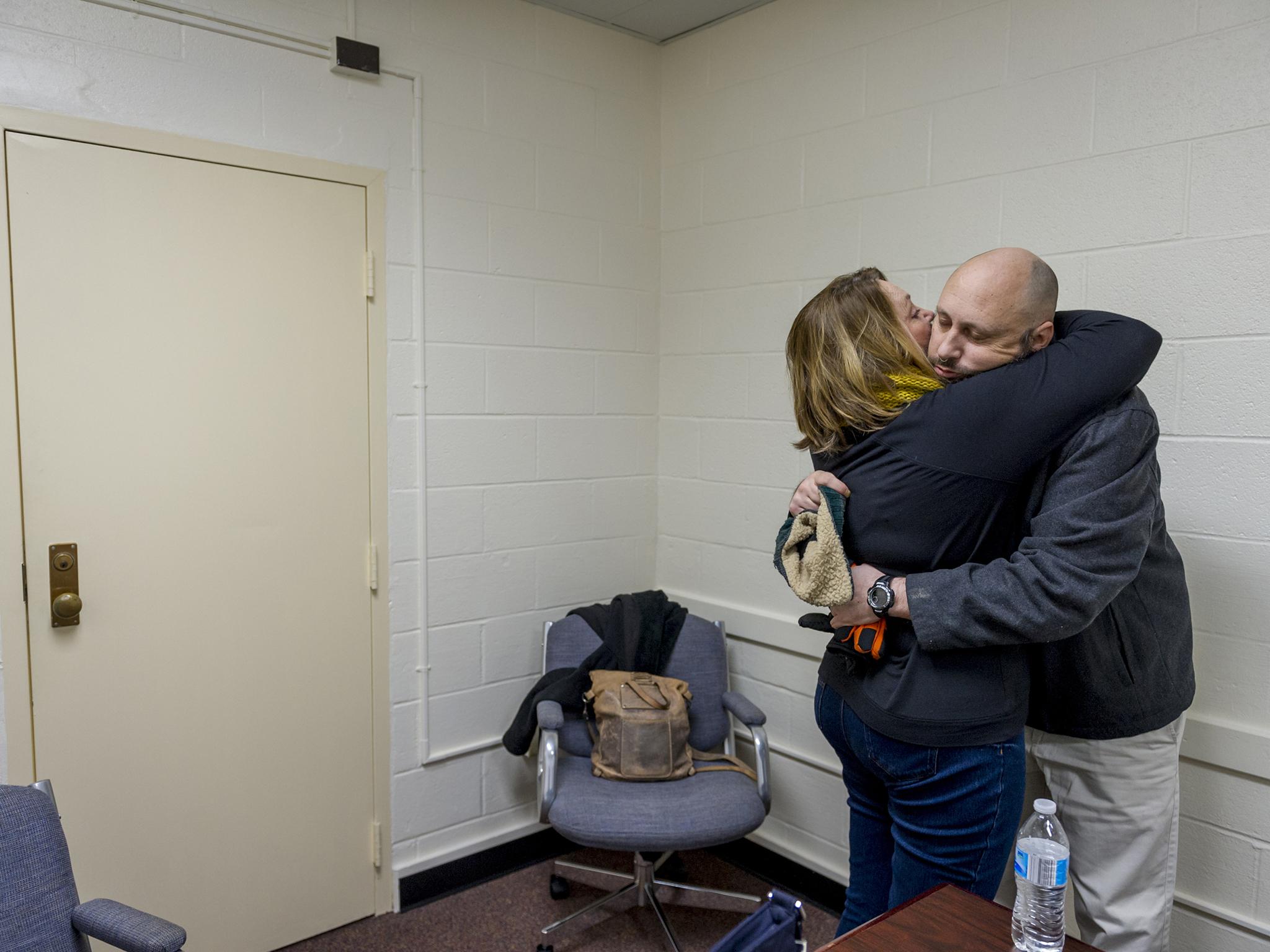
Anita parks in front of an administrative building and heads inside, warning me that Aaron will probably look dishevelled and could be in a bad mood. Sometimes their visits last an hour; other times, 10 minutes. When Aaron greets us in the entryway, she lets out a quiet gasp. He is wearing khaki pants and a long-sleeved blue V-neck shirt and sports a groomed beard and a freshly shaved head. He hasn’t looked this good in years, she muses later, wondering where those clothes came from and who helped him smarten up.
We gather around a table in a cramped room with white cinder-block walls; a woman from the hospital sits in the corner. “I brought the book,” Anita says, handing Aaron the “Superstar’s Keepsake” album. Aaron, then 41, hunches forward, flips open the cover and looks at the headlines.
“Backup QB becomes star.”
“Cougars in title game with Dumsch’s help.”
“Dumsch handles pressure.”
Aaron rubs his beard. “This was our team. I miss these guys! I haven’t seen ‘em in years!” he exclaims. Apart from his trembling hands (a side effect of his medication), he seems more like a visitor than a patient, with his casual tone and jovial attitude. When I ask what it was like being crowned homecoming king – once in junior high and again in high school – a smile spreads across his face. “That never shoulda happened!” he blurts with excitement. “This is the weird thing about me. I go to all these different schools and they appoint me king. I never had enough notoriety to know who these people were! Crown someone else.”
He motions to the photo album, reading another headline aloud: “Peoria has the talent, but Sahuaro has the heart.”
“It’s just crazy, because I was such a good kid in high school. These articles back it up, and then what happened to me after?” He rests his elbows on the table. “I think if some of my teammates and coaches were to find out what happened to me, I think they’d be upset. There’s no way I should have gone through this.”
Aaron takes a long drink of water, then tosses an arm over the back of his chair and tilts towards the wall, exuding the effortless cool his friends remember him for. Living at Springfield isn’t all that bad, he says. He watches Blue Bloods and Wahlburgers. He gets chocolate doughnuts and sodas from the canteen. “You get into a routine. Would I be doing anything more important than this if I weren’t here? Not really.” Anita winces. “I just consider this an upscale jail. I don’t know,” he says, turning to his mother. “I’m not sure what’s gonna happen with me, Mom. I’m just sitting here.”
Anita leans forward. “Something will happen. Something always happens. We’ll just have to – ” she pauses. “Do the best we can.”
Aaron’s leg starts shaking. We’ve been talking for close to half an hour, and he’s growing irritable and rattled. As he sits there, cracking his empty plastic water bottle, I remember Anita telling me how he’ll transform before her eyes, going from seemingly normal to yelling obscenities and claiming she never loved him.
“When you get out, you just go to another program or another system. It’s like they recycle us here, like recycled water,” he says.
Anita tries changing the subject: “Do a lot of people have family members who come visit?”
“Not as much,” Aaron says.
“I’ve never seen another family, ever, since you’ve been here,” she says. “You’ve been here since March and we come every week.”
“That’s a trek for you, Mom.”
“I know,” she says. “We get to see the leaves change. The snow fall. I get to talk to you for a little bit.”
Aaron grows quiet. “This makes no sense,” he says, noticing for the first time that his mother is crying.
“It’s OK,” she whimpers. “We have to find a path for it to make sense. You’re a young man! Heck, I’m a young woman! I’m 65. We’ve got years ahead of us. We have to – I get emotional because I miss you.” She grabs his hand.
“You don’t think I don’t miss you and Dad?” he says.
“I know you do. I know you do.”
“This isn’t right,” Aaron says, his voice suddenly flat and monotone. He looks down at the table, then glares at the hospital staffer who’s been sitting in the corner, quietly, almost motionlessly, since the interview began. “These people are gonna suffer.”
“No! No, no!” Anita pleads, worrying that he might lash out.
“Just listen,” he says, turning to his mother. “Something is gonna happen to me.”
“Stop! Now you’re starting to get that way. OK!” Anita says, each word more assertive than the next. “So, Aaron, let’s take the positive turn. Make the promise. Let’s do the right thing.”
Anita has seen this switch flip before. Aaron will abruptly get upset or start ranting about some non sequitur, and she and Pat will leave early, driving home in silence, each suffering in their own way until one of them asks what’s for dinner or what they’ll do the next day, because life goes on. Now, with tears in her eyes, she looks at Aaron and implores him to calm down.
“It doesn’t matter, Mom.”
“Aaron!” she says firmly. “Somehow we got off track, OK?” She lets out a forceful sigh.
It’s clear the interview is over. A moment later, Aaron turns to me and says in a tone of voice I haven’t heard since the start of our interview, “Thank you, ma’am. Good luck to you, ma’am.” Then he and Anita stand up and fall into an embrace. As she whispers into his ear, he closes his eyes and listens, burying his head in her arms. After a few minutes, he puts on his coat and turns to leave.
In the year to come, Aaron will move to three different wards, but he won’t leave, and his condition will remain the same. Meanwhile, Anita will focus on learning “to love him better”, as she put it to me a few months ago. “My goals may not have been reached for what I thought they’d be, like a cure or a family for him or a home, but the goal for him now is that he’s safe. He’ll never be on the streets. We’ve padded the path so he can function when we are not here.” It took Aaron getting into the criminal-justice system for this to happen, but at least the family now has a plan for the future – and her daughters, Anita notes, “will not have to assume that burden”.
For now, though, on this autumn day at Springfield, Anita watches Aaron walk out, then collapses back in her chair, face wet with tears. “It’s an emotional roller coaster all the time,” she says. “You look at your children, and you never dream this is going to be their fate.” She shakes her head. “Never.”
The Washington Post
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments